Dental Code Membranes
Dental code membranes have revolutionized the field of dentistry, offering innovative solutions for tissue and bone regeneration. These specialized barriers play a critical role in procedures such as guided tissue regeneration (GTR), guided bone regeneration (GBR), and periodontal surgery. As dental professionals strive to achieve optimal patient outcomes, the use of dental membranes has become increasingly prevalent.
This article delves into the world of dental code membranes, exploring their history, types, applications, and the latest advancements in the field. Whether you’re a dental practitioner, researcher, or simply curious about modern dentistry, this comprehensive guide will provide you with valuable insights into this fascinating topic.

2. Understanding Dental Code Membranes
2.1 What Are Dental Code Membranes?
Dental code membranes are biocompatible barriers used in oral and maxillofacial surgeries to promote tissue and bone regeneration. They are designed to prevent the migration of unwanted cells (such as epithelial cells) into the healing area, allowing specialized cells (like osteoblasts and periodontal ligament cells) to regenerate effectively.
2.2 Historical Development of Dental Membranes
The concept of using membranes in dentistry dates back to the 1980s when researchers discovered the potential of barriers to guide tissue regeneration. Early membranes were made from non-resorbable materials like polytetrafluoroethylene (PTFE). Over time, advancements in material science led to the development of resorbable membranes, which eliminated the need for a second surgical procedure to remove the barrier.
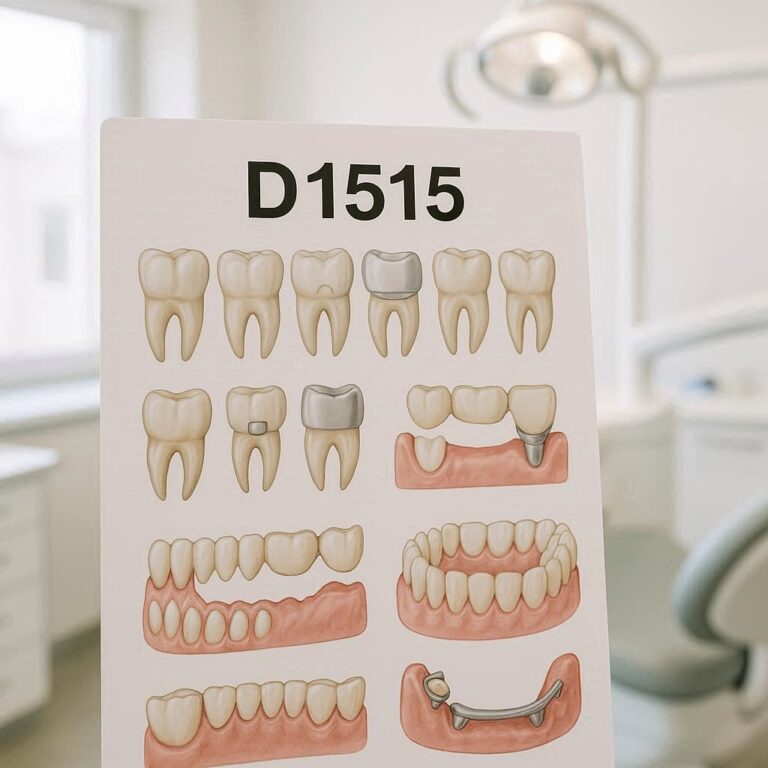
2.3 Types of Dental Membranes
Dental membranes can be broadly categorized into two types:
- Resorbable Membranes: Made from materials like collagen or synthetic polymers, these membranes gradually dissolve in the body.
- Non-Resorbable Membranes: Typically made from PTFE or titanium, these membranes require removal after the healing process.
3. Applications of Dental Code Membranes in Modern Dentistry
3.1 Guided Tissue Regeneration (GTR)
GTR is a technique used to regenerate periodontal tissues lost due to disease. Dental membranes act as barriers to prevent epithelial cells from invading the healing site, allowing periodontal ligament cells to regenerate.
3.2 Guided Bone Regeneration (GBR)
GBR is commonly used in implantology to rebuild bone structures. Membranes create a protected space for bone cells to grow, ensuring successful implant placement.
3.3 Periodontal Surgery
In periodontal surgery, membranes are used to treat defects caused by gum disease, promoting the regeneration of both soft and hard tissues.
3.4 Implantology
Dental membranes are essential in implantology, particularly in cases where bone grafting is required. They help maintain the integrity of the graft and support new bone formation.
4. Materials Used in Dental Code Membranes
4.1 Resorbable vs. Non-Resorbable Membranes
| Property | Resorbable Membranes | Non-Resorbable Membranes |
|---|---|---|
| Material | Collagen, Polylactic Acid | PTFE, Titanium |
| Removal Required | No | Yes |
| Healing Time | Shorter | Longer |
| Cost | Generally Lower | Higher |
4.2 Synthetic vs. Biological Materials
Synthetic membranes offer consistency and predictability, while biological membranes (e.g., collagen) provide better biocompatibility and integration with natural tissues.
4.3 Key Properties of Ideal Dental Membranes
- Biocompatibility
- Mechanical strength
- Ease of handling
- Controlled resorption rate
5. Clinical Techniques and Procedures
5.1 Pre-Surgical Planning
Proper planning, including imaging and patient assessment, is crucial for successful membrane placement.
5.2 Membrane Placement Techniques
The membrane must be carefully positioned to cover the defect and secured to prevent movement during healing.
5.3 Post-Surgical Care and Monitoring
Patients should follow strict oral hygiene practices and attend follow-up appointments to monitor healing progress.
6. Advantages and Limitations of Dental Code Membranes
6.1 Benefits of Using Dental Membranes
- Enhanced tissue and bone regeneration
- Reduced healing time
- Improved outcomes in complex cases
6.2 Common Challenges and Complications
- Membrane exposure
- Infection
- Inadequate integration
7. Innovations in Dental Code Membranes
7.1 Nanotechnology in Membrane Development
Nanotechnology has enabled the creation of membranes with enhanced properties, such as improved strength and controlled drug release.
7.2 3D-Printed Membranes
3D printing allows for the customization of membranes to fit individual patient anatomy, improving outcomes.
7.3 Smart Membranes with Drug Delivery Systems
Smart membranes can release antibiotics or growth factors directly to the surgical site, reducing the risk of infection and promoting healing.
8. Future Trends in Dental Code Membranes
8.1 Personalized Dental Membranes
Advancements in digital dentistry and 3D printing will enable the creation of patient-specific membranes.
8.2 Integration with Digital Dentistry
Digital tools like CAD/CAM will streamline the design and fabrication of dental membranes.
8.3 Sustainability in Membrane Production
Eco-friendly materials and manufacturing processes will become a focus in the development of dental membranes.
9. Case Studies and Real-World Applications
(Include detailed case studies with images and outcomes.)
10. FAQs
Q1: What is the difference between resorbable and non-resorbable membranes?
A: Resorbable membranes dissolve over time, while non-resorbable membranes require surgical removal.
Q2: How long does it take for a dental membrane to resorb?
A: Resorption time varies depending on the material but typically ranges from 4 to 6 months.
Q3: Are dental membranes safe?
A: Yes, dental membranes are biocompatible and widely used in clinical practice.
11. Conclusion
Dental code membranes have transformed modern dentistry, offering innovative solutions for tissue and bone regeneration. With ongoing advancements in materials and technology, the future of dental membranes looks promising, paving the way for personalized and sustainable solutions.
12. Additional Resources
- American Academy of Periodontology
- Journal of Dental Research
- International Journal of Oral Implantology