dental codes for procedures implants aetna insurance
Dental implants have revolutionized the field of restorative dentistry, offering patients a permanent solution for missing teeth. However, navigating the complexities of dental codes and insurance coverage can be overwhelming. For those with Aetna insurance, understanding the specific codes and coverage details for dental implants is crucial to maximizing benefits and minimizing out-of-pocket expenses.
This comprehensive guide delves into the world of dental codes for implant procedures, focusing on Aetna insurance. Whether you’re a patient seeking clarity or a dental professional looking to streamline billing processes, this article provides detailed insights into Aetna’s coverage policies, accepted codes, and tips for ensuring successful claims.
Dental Codes for Procedures: Implants and Aetna Insurance Providers
Understanding Dental Codes
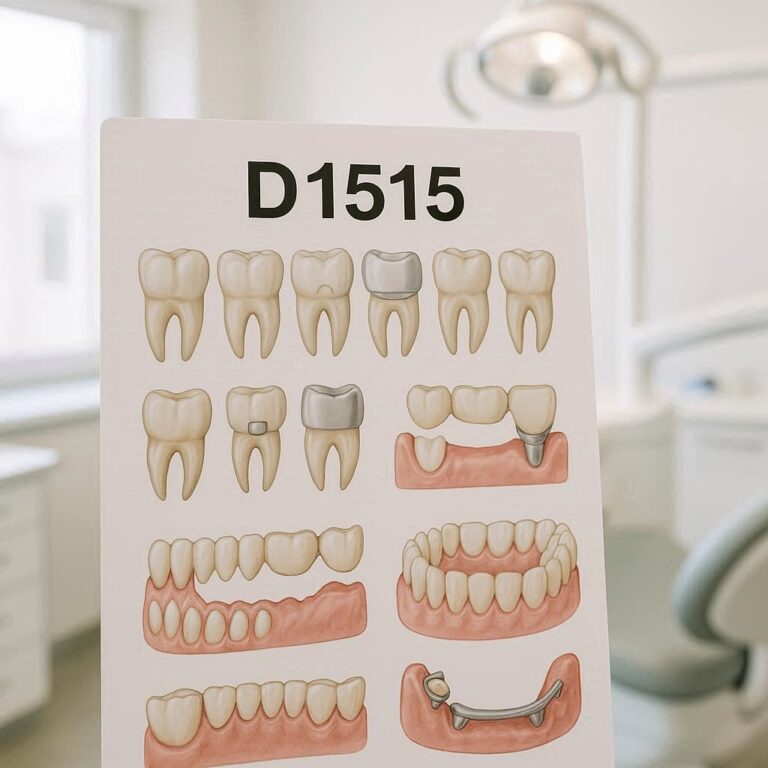
Dental procedures are categorized using Current Dental Terminology (CDT) codes, which are standardized codes maintained by the American Dental Association (ADA). These codes ensure uniformity in billing and insurance claims. For dental implants, specific codes are used to describe each stage of the procedure, from the initial consultation to the final placement of the crown.
Aetna Insurance Providers
Aetna is one of the largest health insurance providers in the United States, offering a range of dental plans. These plans vary in coverage levels, from basic preventive care to major restorative procedures like dental implants. It’s essential to verify whether your specific Aetna plan covers implants, as not all plans include this benefit.
Key Points to Consider:
- Plan Types: Aetna offers PPO, DMO, and indemnity plans. PPO plans typically provide more flexibility in choosing providers but may have higher out-of-pocket costs.
- In-Network vs. Out-of-Network: Staying in-network can significantly reduce costs, as Aetna has negotiated rates with participating dentists.
- Pre-Authorization: Many Aetna plans require pre-authorization for implant procedures to ensure coverage.
Dental Codes for Procedures: Implants and Aetna Insurance Coverage
Coverage for Dental Implants
Aetna’s coverage for dental implants depends on the plan type and the reason for the procedure. While some plans cover implants for cosmetic reasons, most provide coverage only for medically necessary cases, such as tooth loss due to injury or disease.
Common Coverage Scenarios:
- Single Tooth Replacement: Coverage for a single implant and crown.
- Multiple Teeth Replacement: Coverage for bridges or multiple implants.
- Full Mouth Reconstruction: Coverage for implant-supported dentures.
Limitations and Exclusions
- Waiting Periods: Some plans impose waiting periods before covering major procedures.
- Annual Maximums: Aetna plans often have annual maximums, which may not cover the full cost of implants.
- Alternative Benefits: If implants are deemed cosmetic, Aetna may offer alternative benefits for less expensive procedures like dentures.
Dental Codes for Procedures: Implants and Aetna Insurance List
Commonly Used CDT Codes for Implants
Below is a table of frequently used dental codes for implant procedures and their descriptions:
| CDT Code | Description |
|---|---|
| D6010 | Surgical placement of implant body |
| D6056 | Prefabricated abutment |
| D6057 | Custom abutment |
| D6058 | Abutment supported porcelain/ceramic crown |
| D6059 | Abutment supported porcelain fused to metal crown |
| D6060 | Abutment supported cast metal crown |
| D6104 | Bone graft at the time of implant placement |
| D6190 | Radiographic/surgical guide |
How Aetna Uses These Codes
Aetna uses these codes to determine the level of coverage for each stage of the implant process. For example, the surgical placement of the implant body (D6010) may be covered at 50%, while the crown (D6058) may be covered at 80%.
Dental Codes for Procedures: Implants and Aetna Insurance Accepted
Ensuring Your Procedure is Covered
To avoid unexpected costs, follow these steps:
- Verify Coverage: Contact Aetna to confirm your plan’s coverage for implants.
- Obtain Pre-Authorization: Submit a treatment plan to Aetna for approval before proceeding.
- Choose an In-Network Provider: This ensures you receive the maximum benefits.
- Review Your Explanation of Benefits (EOB): After the procedure, check your EOB to confirm the amount covered by Aetna.
Tips for Successful Claims
- Accurate Coding: Ensure your dentist uses the correct CDT codes.
- Detailed Documentation: Provide X-rays, photos, and a detailed treatment plan.
- Follow Up: If a claim is denied, appeal with additional documentation.
Conclusion
Navigating dental codes and insurance coverage for implants can be complex, but understanding Aetna’s policies and procedures can save you time and money. By verifying coverage, obtaining pre-authorization, and working with in-network providers, you can ensure a smooth process and maximize your benefits.
FAQs
1. Does Aetna cover dental implants?
Yes, but coverage varies by plan. Most plans cover implants for medically necessary reasons, such as tooth loss due to injury or disease.
2. What is the average cost of a dental implant with Aetna insurance?
The cost depends on your plan’s coverage level. On average, patients pay between 1,000and1,000and3,000 out-of-pocket per implant after insurance.
3. How do I find an in-network dentist for implants?
Use Aetna’s online provider directory or contact customer service for a list of in-network dentists.
4. What if my claim is denied?
You can appeal the decision by submitting additional documentation, such as X-rays and a detailed treatment plan.
Additional Resources
- Aetna Dental Insurance Plans
- American Dental Association (ADA) CDT Codes
- Guide to Dental Implants by the American Academy of Implant Dentistry