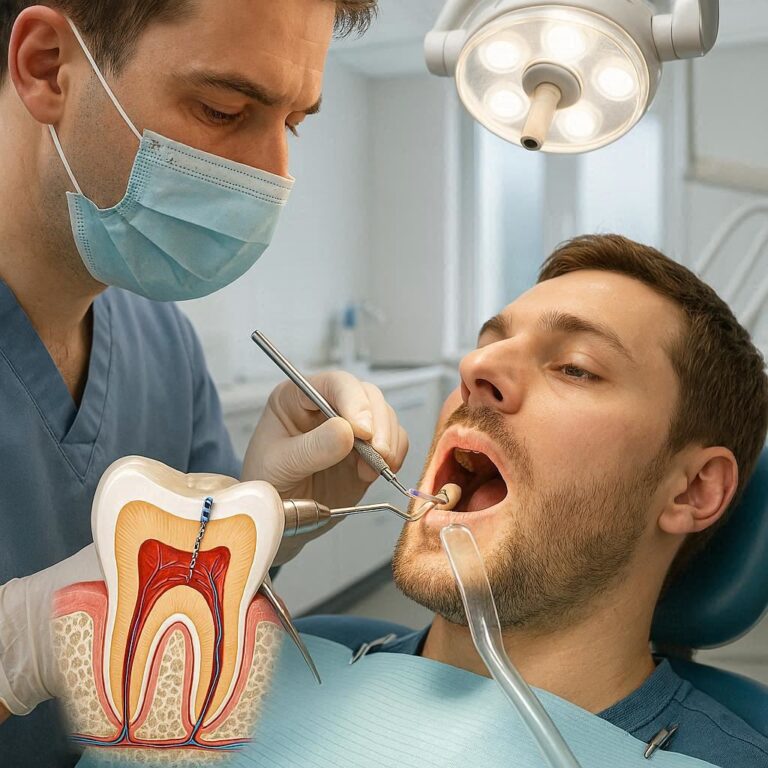
dental Code D7550
The landscape of dental procedures is vast and intricate, governed by a detailed system of codes that classify every intervention from routine cleanings to complex surgical reconstructions. Among these is D7550, a code that, while not as commonly discussed as fillings or extractions, represents a critical procedure in oral and maxillofacial surgery: the partial ostectomy or sequestrectomy for the removal of non-vital bone. This article will navigate the complexities surrounding D7550, exploring its clinical significance, the conditions necessitating the procedure, the surgical process, and the critical aspects of its classification and billing. Understanding D7550 offers valuable insight into the management of serious bone pathology within the oral cavity and surrounding structures.
1. Introduction: The Importance of Understanding Dental Codes
In the realm of healthcare, precision is paramount. This is especially true in dentistry, where a standardized system of codes, known as Current Dental Terminology (CDT), provides a universal language for documenting procedures, communicating with insurance providers, and tracking treatment outcomes. Each code represents a specific service, ensuring clarity and consistency across practices and payers. While codes like D0120 for a periodic oral evaluation or D1110 for adult prophylaxis are widely recognized due to their routine nature, others, such as D7550, pertain to more specialized surgical interventions. For patients, understanding these codes can demystify treatment plans and billing statements. For dental professionals, accurate coding is essential for proper documentation, successful insurance claims, and maintaining a clear record of the care provided. D7550 falls within the surgical section of the CDT codes, specifically addressing conditions that affect the vitality and health of bone tissue in the oral and maxillofacial region.
2. Deciphering D7550: Definition and Context
The code D7550 is officially described as “Partial ostectomy/sequestrectomy for removal of non-vital bone.” To fully grasp this definition, we must break down its components. “Ostectomy” refers to the surgical removal of bone, while “sequestrectomy” specifically denotes the removal of a sequestrum – a piece of dead bone that has become separated from healthy bone during the process of necrosis. “Non-vital bone” indicates bone tissue that is no longer living, typically due to compromised blood supply or overwhelming infection. Therefore, D7550 covers procedures where a surgeon carefully removes a portion of this deceased bone tissue.
This code is situated within the D7000-D7999 series of CDT codes, which are dedicated to Oral and Maxillofacial Surgery procedures. This section encompasses a wide array of surgical interventions, including extractions, biopsies, cyst and tumor removals, fracture management, and procedures on bone. The placement of D7550 within this category underscores its nature as a surgical procedure involving the bone structure of the jaw or face. Unlike simple tooth extractions (D7140-D7250) which primarily involve removing a tooth, D7550 specifically targets the removal of diseased bone itself, often as a consequence of prior infections, trauma, or certain medical conditions.
3. Clinical Indications: When is D7550 Necessary?
The need for a partial ostectomy or sequestrectomy arises when a localized area of bone tissue in the oral or maxillofacial region loses its vitality and becomes necrotic. This non-vital bone cannot heal and can serve as a persistent source of infection, pain, and dysfunction. Several conditions can lead to this state, making D7550 a necessary intervention in specific clinical scenarios.
One of the most common indications for D7550 is osteomyelitis. This is an inflammation of the bone or bone marrow, usually caused by infection. In chronic osteomyelitis, the infection can lead to impaired blood flow and subsequent bone necrosis, forming sequestra. These dead bone fragments act as foreign bodies and reservoirs of infection, preventing resolution of the disease. Surgical removal of the sequestrum (sequestrectomy) and sometimes surrounding affected bone (partial ostectomy) is crucial to eliminate the infection and allow the remaining healthy bone to heal.
Another significant indication is osteonecrosis, which is the death of bone tissue due to a lack of blood supply. While osteonecrosis can occur in various bones throughout the body, it can also affect the jawbones. Medication-related osteonecrosis of the jaw (MRONJ) is a recognized complication associated with certain medications, particularly bisphosphonates and some anti-angiogenic drugs, used in the treatment of osteoporosis and certain cancers. In cases of established MRONJ where a portion of bone has become exposed and necrotic, surgical debridement and removal of the non-vital bone (partial ostectomy/sequestrectomy) may be required to manage the condition, control infection, and alleviate symptoms.
Trauma can also lead to localized areas of bone necrosis if the blood supply is severely compromised. While immediate management of fractures aims to restore blood flow, in some cases, a segment of bone may still lose vitality and require removal later. Radiation therapy to the head and neck region can also induce osteoradionecrosis (ORN), a serious complication where bone tissue dies due to damage from radiation. ORN can lead to exposed bone, pain, infection, and pathological fractures. Surgical debridement, often involving partial ostectomy and sequestrectomy, is a key component in the management of ORN, particularly in advanced cases.
In summary, D7550 is indicated for conditions characterized by localized bone necrosis or the presence of sequestra, most notably:
- Chronic Osteomyelitis
- Medication-Related Osteonecrosis of the Jaw (MRONJ)
- Osteoradionecrosis (ORN)
- Post-traumatic or post-surgical bone necrosis
The decision to perform this procedure is based on clinical examination, radiographic findings (such as areas of radiolucency or visible sequestra on X-rays or CT scans), and the patient’s symptoms.
(Image Description: A diagram showing a cross-section of jawbone with an area of darkened, irregular bone representing a sequestrum surrounded by inflamed tissue.)
4. The Pathophysiology: Understanding Non-Vital Bone
To appreciate the necessity of D7550, it’s helpful to understand why bone becomes non-vital. Healthy bone is a dynamic tissue, constantly being remodeled through a balance of bone resorption (breakdown by osteoclasts) and bone formation (building by osteoblasts). This process relies heavily on a robust blood supply that delivers nutrients and oxygen and removes waste products.
When the blood supply to a section of bone is severely compromised or completely cut off, the bone cells (osteocytes, osteoblasts, and osteoclasts) die. This can happen due to several mechanisms:
- Infection: Bacteria can invade bone tissue, causing inflammation and thrombosis (blood clot formation) in the blood vessels supplying the bone. This cuts off the blood supply, leading to necrosis. The body’s immune response attempts to wall off the infection, sometimes leading to the formation of an involucrum (new bone formation around the dead bone) and a cloaca (a channel allowing pus to drain), with the dead bone fragment becoming a sequestrum.
- Trauma: Severe fractures, crush injuries, or surgical procedures can damage or sever the blood vessels supplying a bone segment. If collateral circulation is insufficient, necrosis can occur.
- Radiation: High-dose radiation therapy damages the cells and blood vessels in the irradiated area, including bone. This microvascular damage reduces blood flow over time, making the bone susceptible to necrosis, especially if further challenged by trauma or infection (like tooth extraction in a radiated field).
- Medications: Certain medications, particularly antiresorptive agents like bisphosphonates, can suppress bone remodeling. While this is beneficial for conditions like osteoporosis, in some individuals, coupled with local factors like trauma or infection, it can impair the bone’s ability to repair itself and respond to insult, leading to osteonecrosis. Anti-angiogenic drugs used in cancer treatment can also contribute by inhibiting the formation of new blood vessels needed for bone repair.
Non-vital bone is essentially dead tissue within a living system. It is prone to infection, cannot contribute to structural integrity, and can cause chronic pain and inflammation. Removing this non-vital bone is a necessary step to control infection, eliminate the source of irritation, and create a favorable environment for the healing of surrounding vital tissues.
5. Pre-Surgical Assessment and Planning
Before performing a partial ostectomy or sequestrectomy, a thorough pre-surgical assessment is crucial. This process involves:
- Detailed Medical History Review: Identifying underlying medical conditions, medications (especially bisphosphonates or immunosuppressants), history of radiation therapy, and risk factors for impaired healing.
- Comprehensive Dental History and Clinical Examination: Evaluating the affected area, noting signs of infection (swelling, redness, pus), pain levels, presence of exposed bone, mobility of bone segments, and the overall oral hygiene status.
- Radiographic Imaging: Essential for visualizing the extent of the non-vital bone, identifying sequestra, assessing the relationship to vital structures (nerves, blood vessels, adjacent teeth), and evaluating the health of the surrounding bone. Periapical X-rays, panoramic radiographs, and Cone Beam Computed Tomography (CBCT) scans are commonly used. CBCT provides detailed 3D images, which are particularly valuable for surgical planning in complex cases.
- Laboratory Tests: May be required to assess for systemic infection (e.g., complete blood count, C-reactive protein) or to evaluate the patient’s overall health status, especially if sedation or general anesthesia is planned.
- Consultation with Specialists: Depending on the underlying cause of the non-vital bone (e.g., ONJ, ORN), collaboration with the patient’s physician or oncologist may be necessary to optimize systemic health before surgery.
Based on the assessment, the surgeon develops a detailed surgical plan. This includes determining the extent of bone to be removed, the surgical approach (intraoral or extraoral), the type of anesthesia, and planning for potential reconstruction if a significant bone defect will result from the removal. The goal is to remove all non-vital bone while preserving as much healthy tissue as possible and minimizing morbidity.
(Image Description: A panoramic X-ray showing an area of irregular bone density in the mandible indicative of osteonecrosis or osteomyelitis, with a distinct sequestrum visible.)
6. The Surgical Procedure: Partial Ostectomy/Sequestrectomy
The surgical procedure for D7550, partial ostectomy/sequestrectomy, is a delicate operation performed by an oral and maxillofacial surgeon. While the specific steps may vary depending on the location and extent of the non-vital bone, the general process involves several key stages:
- Anesthesia: The procedure can be performed under local anesthesia, conscious sedation, or general anesthesia, depending on the complexity, extent, and patient factors. Adequate anesthesia is critical for patient comfort and surgical access.
- Incision and Flap Reflection: An incision is carefully made in the gum tissue (mucosa) overlying the affected bone. A mucoperiosteal flap, which includes the gum tissue and the underlying periosteum (the membrane covering the bone), is then carefully lifted and retracted to expose the underlying bone. The design of the flap is crucial to ensure adequate access to the surgical site and to preserve blood supply for proper healing.
- Identification and Isolation of Non-Vital Bone: The surgeon carefully identifies the boundaries between the non-vital (sequestrum or necrotic bone) and vital bone. Non-vital bone often appears different visually and can sometimes be detected by probing. Radiographic images serve as a guide.
- Removal of Non-Vital Bone (Sequestrectomy/Ostectomy): Using specialized surgical instruments, such as bone chisels, osteotomes, or rotary burs, the surgeon meticulously separates and removes the non-vital bone tissue. In a sequestrectomy, the separated sequestrum is carefully lifted out. In a partial ostectomy, a portion of necrotic bone still attached to vital bone is surgically cut away. The goal is to remove all diseased bone until healthy, bleeding bone is encountered.
- Debridement and Irrigation: The surgical site is thoroughly cleaned to remove any remaining debris, infected tissue, or small bone fragments. Copious irrigation with sterile saline or an antiseptic solution is performed to flush out contaminants.
- Assessment of Surgical Site: The surgeon assesses the remaining bone margins to ensure all non-vital bone has been removed and that the vital bone edges are smooth. The surrounding soft tissues are also inspected.
- Closure: The mucoperiosteal flap is repositioned to cover the exposed bone defect. Sutures are placed to close the incision, ensuring proper soft tissue coverage and tension-free closure to promote healing and prevent complications. In some cases, a drain may be placed to manage post-operative swelling and bleeding.
The procedure requires precision and careful surgical technique to minimize trauma to surrounding vital structures, such as nerves (like the inferior alveolar nerve in the mandible) and blood vessels.
(Image Description: A drawing illustrating the surgical removal of a bone fragment (sequestrum) from the jawbone using surgical instruments.)
7. Anesthesia and Pain Management
Effective anesthesia is paramount during a partial ostectomy or sequestrectomy to ensure patient comfort and facilitate a smooth surgical procedure. The choice of anesthesia depends on several factors, including the extent and location of the non-vital bone, the patient’s medical status, anxiety level, and the surgeon’s preference.
- Local Anesthesia: For smaller, more localized areas of non-vital bone removal, local anesthesia may be sufficient. This involves injecting an anesthetic agent directly into the surgical area, numbing the nerves and preventing pain sensation. The patient remains awake and aware during the procedure.
- Conscious Sedation: Also known as moderate sedation, this involves administering medications (often intravenously or orally) that induce a state of relaxation and reduced awareness. The patient is still able to respond to verbal commands but is less anxious and may have little memory of the procedure. Local anesthesia is typically still used in conjunction with conscious sedation to ensure the surgical site is numb.
- General Anesthesia: For more extensive procedures, complex anatomy, or for patients with significant anxiety or medical complexities, general anesthesia may be recommended. Under general anesthesia, the patient is completely unconscious and has no awareness or sensation of the procedure. This requires the services of an anesthesiologist or nurse anesthetist and is typically performed in a hospital or accredited outpatient surgical center.
Post-operative pain management is also a critical aspect of care. The surgeon will prescribe appropriate pain medication, which may include over-the-counter analgesics or prescription opioid pain relievers, depending on the anticipated level of discomfort. Anti-inflammatory medications are often recommended to reduce swelling. Patients are instructed on how to manage pain and swelling and when to contact the office if pain is not controlled.
8. Instrumentation and Techniques
Performing a partial ostectomy or sequestrectomy requires a specific set of surgical instruments designed for working with bone. These include:
- Scalpels: For making precise incisions in the soft tissue.
- Periosteal Elevators: Used to carefully lift the mucoperiosteal flap away from the bone.
- Retractors: To hold the soft tissues out of the way, providing clear visibility of the surgical field.
- Bone Chisels and Mallets: Traditional instruments used to cut or shape bone.
- Osteotomes: Similar to chisels, used for cutting bone.
- Bone Rongeurs: Pliers-like instruments used for nipping away small pieces of bone.
- Bone Files: Used to smooth sharp edges of bone.
- Rotary Instruments (Drills and Burs): High-speed or low-speed handpieces with specialized burs are commonly used for precise bone cutting and shaping. Irrigation with sterile saline is essential when using rotary instruments on bone to prevent overheating and damage.
- Curettes: For removing granulation tissue, infected material, or small fragments from the bone cavity.
- Surgical Suction: To remove blood, irrigation solution, and debris from the surgical field.
- Suture Materials and Needles: For closing the soft tissue incision.
The technique employed by the surgeon will depend on the specific clinical situation, the location and size of the non-vital bone, and the surgeon’s experience. Careful planning and execution are essential to minimize complications and achieve a successful outcome. Techniques may include block resection (removing a solid block of bone), piecemeal removal of a sequestrum, or saucerization (creating a shallow, open wound to promote healing from the base).
9. Post-Operative Care and Recovery
Proper post-operative care is crucial for a smooth recovery and to minimize the risk of complications following a partial ostectomy or sequestrectomy. Patients will receive detailed instructions from the surgical team, which typically include:
- Pain Management: Taking prescribed pain medication as directed.
- Swelling Control: Applying ice packs to the external facial area overlying the surgical site, especially in the first 24-48 hours. Keeping the head elevated can also help.
- Bleeding Control: Gentle biting on gauze pads placed over the surgical site, if applicable. Some oozing is normal, but excessive or prolonged bleeding should be reported.
- Oral Hygiene: Maintaining good oral hygiene is important, but gentle care around the surgical site is necessary. Rinsing with warm salt water (a teaspoon of salt in a glass of warm water) several times a day, starting 24 hours after surgery, can help keep the area clean and promote healing. Brushing other areas of the mouth can be done normally.
- Diet: Starting with soft, cool foods and gradually progressing to a regular diet as tolerated. Avoiding hot, spicy, or hard/crunchy foods that could irritate the surgical site is recommended.
- Activity Level: Avoiding strenuous activity for several days to a week after surgery to minimize swelling and bleeding.
- Medications: Completing any prescribed antibiotics to prevent infection and taking other medications as directed.
- Follow-up Appointments: Attending scheduled post-operative appointments so the surgeon can monitor healing, remove sutures (if non-resorbable), and address any concerns.
Recovery time varies depending on the extent of the surgery and the individual patient’s healing capacity. Swelling and bruising are common and usually subside within a week or two. Pain should gradually decrease. Complete healing of the bone defect will take longer, potentially several months.
10. Potential Complications and Their Management
Like any surgical procedure, partial ostectomy and sequestrectomy carry potential risks and complications. While relatively uncommon in the hands of an experienced surgeon, patients should be aware of them:
- Infection: Despite prophylactic antibiotics, infection can occur at the surgical site. Signs include increased pain, swelling, redness, warmth, and pus drainage. Treatment typically involves antibiotics and potentially drainage of the infected area.
- Bleeding: Some post-operative oozing is normal, but excessive or prolonged bleeding may require intervention, such as placing additional sutures or applying pressure.
- Nerve Injury: The proximity of nerves, particularly the inferior alveolar nerve in the mandible (supplying sensation to the lower lip, chin, and teeth) and the lingual nerve (supplying sensation to the tongue), puts them at risk during surgery. Injury can result in temporary or, in rare cases, permanent numbness or altered sensation.
- Delayed Healing or Non-Union: The bone defect may heal slowly or fail to heal properly, especially in patients with compromised healing (e.g., those with uncontrolled diabetes, poor nutrition, or history of radiation).
- Fracture: In cases of extensive bone removal, the remaining bone may be weakened, increasing the risk of a pathological fracture, especially in the mandible.
- Damage to Adjacent Teeth: While care is taken to protect surrounding teeth, they could potentially be damaged during bone removal.
- Orocutaneous or Oroantral Fistula: An abnormal connection between the oral cavity and the skin or the maxillary sinus, respectively, can occur if the surgical site fails to close properly, especially in cases of large defects or compromised tissue.
Managing complications requires prompt recognition and appropriate intervention by the oral surgeon. This may involve additional medications, minor procedures, or, in rare cases, further surgery.
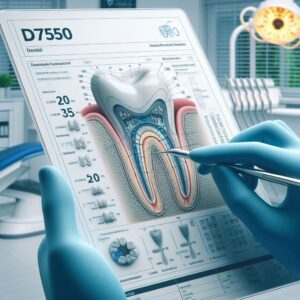
11. Coding, Billing, and Insurance Considerations
Understanding the billing aspects of D7550 is crucial for both dental practices and patients navigating insurance coverage. D7550 falls under the CDT codes for oral surgery and is typically reported per quadrant of the mouth (upper left, upper right, lower left, lower right). However, some payers may require reporting based on the specific anatomical location.
Billing for D7550 requires accurate documentation. The dental claim submitted to the insurance company must include:
- The CDT code D7550.
- The date of the procedure.
- The tooth number(s) or anatomical area involved.
- A detailed narrative or surgical report describing the clinical condition necessitating the procedure, the extent of non-vital bone removed, the surgical technique used, and the findings during surgery. Supporting documentation, such as pre-operative radiographs and clinical photographs, is often required by insurance companies to process the claim and determine medical necessity.
Navigating insurance coverage for D7550 can be complex. While it is a dental procedure, the underlying conditions necessitating it (like osteomyelitis or MRONJ) may be related to systemic health issues. Therefore, there are instances where D7550 may be considered for coverage under a patient’s medical insurance plan, particularly if the condition is deemed medically necessary to treat a systemic disease process. This is known as cross-coding, where the dental procedure code (CDT) is translated into a corresponding medical procedure code (CPT – Current Procedural Terminology) and billed to medical insurance. Common CPT codes that may correspond to D7550 include those for excision of bone in the mandible or maxilla.
(Table 1: Example Cross-Coding Possibilities for D7550)
Note: Cross-coding is complex and depends on the specific clinical scenario, payer policies, and documentation. This table provides potential correspondences and should not be considered definitive billing advice.
Pre-authorization or pre-determination of benefits is often recommended for D7550, especially when billing to medical insurance, to confirm coverage and understand patient financial responsibility (deductibles, copayments, coinsurance). Denial of claims can occur if documentation is insufficient, the procedure is deemed not medically necessary by the payer, or if the policy excludes coverage for the specific condition or procedure. Appeals processes are available if a claim is denied.
12. Related Procedures and Differential Diagnosis
D7550 is part of a suite of surgical codes and must be differentiated from other procedures in the D7000-D7999 series. It’s important to distinguish D7550 from:
- Extractions (D7140-D7250): These codes cover the removal of teeth. While non-vital bone may be present around a tooth requiring extraction, D7550 specifically codes the removal of the bone itself, not the tooth. If both are performed, both codes may be reported with appropriate modifiers and documentation.
- Removal of Foreign Bodies (D7530, D7540, D7560): These codes are for removing non-tissue materials (like broken instruments or displaced restorative materials) from soft tissue, musculoskeletal system, or the maxillary sinus. D7550 is for removing non-vital bone tissue.
- Removal of Cysts or Tumors (D7450-D7471): These codes are for the excision of pathological soft tissue or bone lesions that are not necessarily non-vital bone.
The differential diagnosis for conditions requiring D7550 includes other pathologies that can affect bone, such as primary bone tumors, metastatic lesions, fibrous dysplasia, and certain infectious diseases. Accurate diagnosis through clinical evaluation, imaging, and sometimes biopsy is essential to determine the appropriate treatment and coding.
13. Advances and Future Perspectives
The field of oral and maxillofacial surgery is constantly evolving, with advancements impacting procedures like partial ostectomy and sequestrectomy. Some areas of progress include:
- Advanced Imaging Techniques: Improved resolution and capabilities of CBCT and other imaging modalities allow for more precise identification and mapping of non-vital bone, aiding in surgical planning and minimizing the removal of healthy tissue.
- Minimally Invasive Techniques: Development of smaller instruments and techniques that allow for less extensive surgical access, potentially leading to faster recovery and reduced post-operative complications.
- Biomaterials and Tissue Engineering: Research into using bone graft materials and growth factors to promote healing and regeneration of bone defects following the removal of non-vital bone. This is particularly relevant when significant bone volume is lost.
- Improved Understanding of ONJ and ORN: Ongoing research into the mechanisms of ONJ and ORN is leading to better strategies for prevention, earlier diagnosis, and more effective medical and surgical management protocols.
- Antibiotic Therapies: Development of new antibiotics and strategies for local antibiotic delivery to better control infection in compromised bone.
These advancements aim to improve the predictability of outcomes, reduce patient morbidity, and enhance the overall quality of care for patients requiring the removal of non-vital bone.
14. The Role of the Oral Surgeon
Procedures coded under D7550 are typically performed by oral and maxillofacial surgeons. These specialists undergo extensive training beyond dental school, focusing on the diagnosis and surgical management of diseases, injuries, and defects of the mouth, jaw, face, and skull. Their expertise in bone surgery, anesthesia, and managing complex medical histories makes them uniquely qualified to perform partial ostectomy and sequestrectomy safely and effectively.
Choosing an experienced oral surgeon is crucial for patients requiring this procedure. Their skill and judgment are paramount in accurately diagnosing the condition, developing an appropriate treatment plan, performing the surgery with precision, and managing any potential complications.
(Image Description: A photo of an oral surgeon in a surgical setting, wearing scrubs and gloves, looking at dental radiographs on a light box.)
15. Conclusion
D7550 represents the surgical removal of non-vital bone, a critical procedure for managing conditions like osteomyelitis, osteonecrosis, and osteoradionecrosis. Performed by oral and maxillofacial surgeons, this intervention is essential for eliminating infection, promoting healing, and restoring function. Accurate diagnosis, meticulous surgical technique, and comprehensive post-operative care are key to successful outcomes for patients requiring partial ostectomy or sequestrectomy.
16. Frequently Asked Questions (FAQs)
- Q: What is non-vital bone? A: Non-vital bone is bone tissue that has died, usually due to loss of blood supply or overwhelming infection.
- Q: What causes bone to become non-vital? A: Common causes include severe infections (osteomyelitis), certain medications (like bisphosphonates), radiation therapy to the head and neck, and trauma.
- Q: Is D7550 a common dental procedure? A: No, it is less common than routine procedures like fillings or extractions. It is a specialized surgical procedure performed when specific bone pathology is present.
- Q: Will my insurance cover D7550? A: Coverage varies depending on your specific dental and/or medical insurance plan and the medical necessity of the procedure. Pre-authorization is often recommended.
- Q: What is a sequestrum? A: A sequestrum is a piece of dead bone that has become separated from the surrounding healthy bone.
- Q: Is the procedure painful? A: The procedure is performed under anesthesia to ensure you do not feel pain during the surgery. Some discomfort is expected during the recovery period, which can be managed with prescribed pain medication.
- Q: How long does recovery take? A: Initial recovery, including the reduction of swelling and pain, typically takes 1-2 weeks. Complete bone healing takes several months.
- Q: What are the potential risks of D7550 surgery? A: Risks include infection, bleeding, nerve injury (leading to numbness), delayed healing, and, in rare cases, fracture of the jawbone. Your surgeon will discuss these risks with you.
- Q: Can I eat normally after the surgery? A: You will need to start with a soft diet and gradually advance as tolerated. Avoid hard or crunchy foods that could injure the surgical site.
- Q: Why is a detailed surgical report important for billing? A: The report provides the insurance company with the necessary information to understand the complexity and medical necessity of the procedure, supporting the claim for D7550.
17. Additional Resources (Suggested)
For those seeking further information about D7550, the conditions it treats, or oral surgery in general, consider consulting the following types of resources:
- American Dental Association (ADA): Their website provides information on CDT codes and patient education materials.
- American Association of Oral and Maxillofacial Surgeons (AAOMS): This professional organization offers resources for both patients and professionals regarding oral and maxillofacial surgery procedures and conditions.
- Reputable Medical and Dental Journals: Publications in oral surgery, periodontology, and head and neck surgery may contain in-depth articles on the diagnosis and management of conditions requiring D7550.
- Academic Medical Center Websites: University-affiliated hospitals with oral and maxillofacial surgery departments often have patient information sections explaining common procedures and conditions.
- Your Oral and Maxillofacial Surgeon: Your treating surgeon is the best resource for specific questions about your individual case, treatment plan, and expected recovery.