D7610 Dental Code
1. Introduction: When a Tooth Needs More Than a Simple Goodbye
For many, the thought of a tooth extraction conjures images of a quick, straightforward procedure – a little local anesthetic, a firm pull with forceps, and it’s over. While this is often the case for teeth that are easily accessible and have straightforward root structures, dentistry frequently encounters situations where a tooth’s removal presents a far greater challenge. These aren’t just “extractions”; they are surgical procedures requiring careful planning, advanced techniques, and a deeper understanding of oral anatomy. This is where dental code D7610 comes into play, signifying a level of complexity that goes “beyond the simple pull.” This article delves into the world of D7610, exploring what this code represents, why such procedures are necessary, the intricate steps involved, and what patients can expect when facing a surgical tooth extraction.

2. Decoding D7610: Understanding the Surgical Extraction
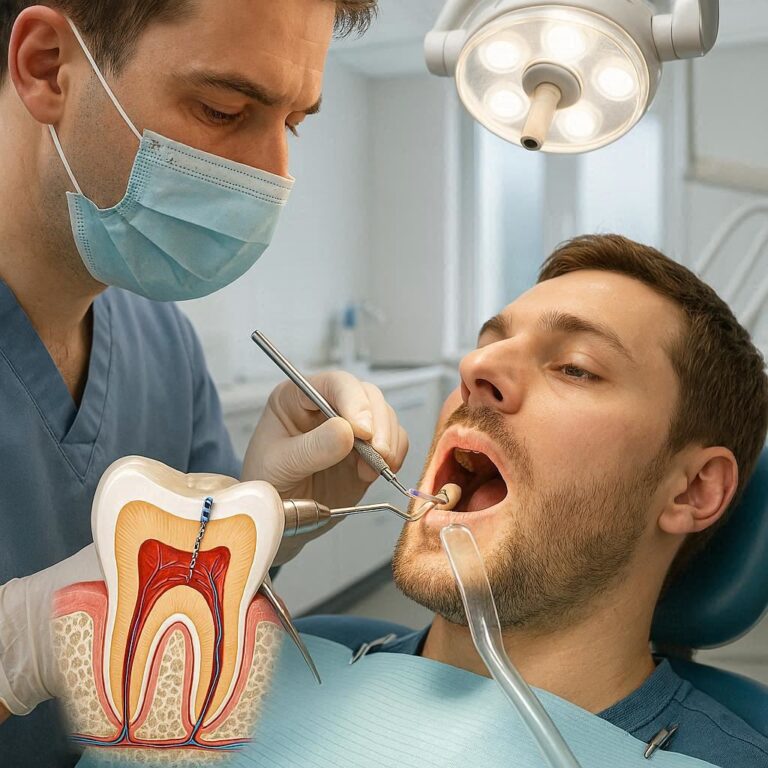
Dental Procedure Code D7610 is a specific descriptor used in the dental coding system (CDT®) to identify a particular type of tooth extraction. Unlike the code for a simple extraction (D7140), D7610 signifies a procedure that is more complex and requires surgical intervention. The key elements that define a D7610 procedure are the necessity of elevating a mucoperiosteal flap and the removal of bone and/or sectioning of the tooth.
Let’s break down these components:
- Mucoperiosteal Flap: The mucoperiosteum is the soft tissue (mucosa) and the underlying connective tissue (periosteum) that covers the bone around the tooth. In a surgical extraction, an incision is made in the gum tissue, and this layer is carefully lifted or “elevated” away from the underlying bone. This provides the dentist or oral surgeon with direct visibility and access to the tooth roots and the surrounding bone, which is often necessary when the tooth is not fully erupted, is impacted, or is surrounded by dense bone.
- Removal of Bone: In many cases requiring a D7610 code, the tooth is embedded in bone or the bone is preventing its removal. This necessitates the careful and controlled removal of a small amount of this supporting bone using specialized dental drills or instruments. This is done to create a pathway for the tooth to be safely extracted without causing excessive trauma. The amount of bone removed is precisely calculated to be the minimum necessary for successful extraction.
- Sectioning of Tooth: Sometimes, the shape or position of the tooth, particularly if it has multiple roots or unusually curved roots, makes it impossible to remove in one piece. In these instances, the tooth is carefully divided into smaller sections using a dental drill. Each section is then removed individually. This technique minimizes trauma to the surrounding bone and tissues and can make the extraction of complex teeth significantly safer and more predictable.
Therefore, a procedure coded as D7610 involves not just the removal of a tooth, but a surgical approach that includes accessing the area by lifting the gum tissue and often involves modifying the surrounding bone or dividing the tooth itself to facilitate its safe removal.
3. The Clinical Imperative: Why Surgical Extraction Becomes Necessary
A tooth extraction categorized under D7610 is not a matter of choice; it’s a clinical necessity dictated by the condition and position of the tooth and the surrounding oral structures. Several scenarios warrant this more involved surgical approach:
-
Impacted Teeth: This is perhaps the most common reason for a D7610 extraction, particularly with wisdom teeth (third molars). An impacted tooth is one that has not fully erupted through the gums and bone. It might be stuck against another tooth, growing at an angle, or completely encased in bone. Removing an impacted tooth invariably requires lifting a flap to access it and often involves removing overlying bone and sectioning the tooth.
- Example Scenario: A patient presents with pain and swelling around their lower wisdom tooth. Radiographs reveal the tooth is horizontally impacted, pressing against the adjacent second molar. A D7610 procedure is necessary to access, free, and remove this tooth.
-
Severely Fractured Teeth: When a tooth is broken below the gum line or has root fractures, it cannot be simply gripped and pulled. The remaining tooth structure may be fragile or deeply embedded. Surgical access via a flap and potentially bone removal might be needed to carefully retrieve the fragments.
- Example Scenario: A tooth has fractured vertically, extending down into the root. Attempting a simple extraction would likely cause further damage. A surgical approach is needed to expose the roots and remove the fractured portions.
-
Teeth with Complex Root Anatomy: Teeth with unusually shaped, multiple, divergent, or severely curved roots can be incredibly difficult to remove with standard forceps. These complex root structures can be firmly anchored in the bone. Sectioning the tooth allows each root or portion to be removed separately, reducing the risk of root fracture or damage to the jawbone.
- Example Scenario: An upper molar has three widely spread roots that are tightly embedded in the maxillary bone. To remove it safely, the dentist might section the tooth into three parts, removing each root individually after flap elevation and potentially some bone contouring.
-
Teeth Involved in Pathology: Teeth associated with cysts, tumors, or other pathological lesions may require a D7610 extraction as part of a broader surgical procedure to remove the pathology and the affected tooth. The extent of bone removal can be more significant in these cases to ensure complete excision of the lesion.
- Example Scenario: An X-ray reveals a large cyst surrounding the roots of a lower premolar. Removing the cyst requires surgical access, which will also involve the extraction of the affected tooth, typically coded as D7610.
-
Failed Root Canal Treated Teeth: Although root canal treatment aims to save a tooth, sometimes the treatment fails due to persistent infection, complex anatomy, or root fractures. If retreatment or surgical intervention (like an apicoectomy) is not feasible or successful, the tooth may need to be extracted. These teeth can be brittle or have post/core buildups, making a surgical approach necessary.
- Example Scenario: A tooth that had a root canal years ago becomes infected again, and attempts to retreat it are unsuccessful. The tooth is deemed non-restorable and requires extraction, likely a surgical one due to its history and potential for complexity.
-
Teeth with Ankylosis: Ankylosis is a condition where the tooth root fuses directly to the jawbone, without the cushioning periodontal ligament. Ankylosed teeth are rigid and cannot be loosened with traditional extraction techniques. Surgical intervention, including bone removal around the fused root, is required for their removal.
- Example Scenario: A primary tooth fails to exfoliate (fall out) and remains in the arch past its expected time. Radiographs confirm ankylosis. A surgical extraction is needed to remove the fused tooth.
In essence, D7610 procedures are indicated when the tooth’s position, structure, or surrounding environment makes a simple, non-surgical extraction either impossible or significantly risky for the patient and the surrounding tissues.
4. Anatomy of a Surgical Extraction: A Step-by-Step Journey
A surgical tooth extraction coded as D7610 is a meticulously planned and executed procedure. While variations exist depending on the specific case, the general steps involved are as follows:
Step 1: Anesthesia The procedure begins with administering local anesthesia to numb the tooth and the surrounding gum and bone. This ensures the patient is comfortable and feels no pain during the extraction. In more complex cases or for anxious patients, sedation (ranging from nitrous oxide to intravenous sedation) may also be used to help the patient relax.
(Image Suggestion: A diagram showing the injection of local anesthetic into the gum tissue around a tooth.)
Step 2: Incision and Flap Elevation Once the area is numb, a precise incision is made in the gum tissue around the tooth. The design of the incision is crucial and is planned based on the tooth’s location and the anticipated needs for access and closure. Specialized instruments, like periosteal elevators, are then used to carefully lift the mucoperiosteal flap away from the underlying bone. This exposes the tooth root(s) and the surrounding bone that might be obstructing removal.
Step 3: Bone Removal (Osteotomy) If necessary, a small amount of bone surrounding the tooth is carefully removed. This process, called osteotomy, is typically performed using a dental handpiece (drill) with sterile saline irrigation to keep the bone cool and prevent damage. The amount of bone removed is the minimum required to create a clear path for the tooth to be extracted.
Step 4: Tooth Sectioning (Odontotomy) If the tooth’s anatomy or position requires it, the tooth is sectioned. Using a dental drill, the crown and/or roots are carefully divided into smaller pieces. This allows for the removal of each section individually, reducing stress on the jawbone and minimizing the risk of complications like root fracture or excessive bone removal.
Step 5: Tooth Removal With access gained and any necessary bone removed or tooth sectioning completed, specialized instruments like elevators and forceps are used to gently loosen and remove the tooth or its sections from the socket. Care is taken to apply controlled forces to minimize trauma to the surrounding tissues.
Step 6: Socket Management After the tooth is removed, the tooth socket is carefully inspected. Any remaining bone fragments, infected tissue, or foreign debris are removed. The socket may be gently irrigated with sterile saline. In some cases, bone grafting material may be placed in the socket to preserve the bone volume, particularly if the patient is considering future tooth replacement options like dental implants.
Step 7: Closure The mucoperiosteal flap is then carefully repositioned back over the socket. Sutures (stitches) are typically used to close the incision and hold the gum tissue in place. Sutures help to control bleeding, protect the healing socket, and promote proper tissue regeneration. Most sutures used in the mouth are dissolvable and will disappear on their own within a week or two.
Step 8: Post-Operative Instructions Detailed post-operative instructions are provided to the patient regarding pain management, swelling control, diet, oral hygiene, and what to do in case of complications.
This step-by-step process highlights the surgical nature of a D7610 procedure, emphasizing the planning, precision, and various techniques that differentiate it from a simple extraction.
5. Managing Comfort: Anesthesia and Pain Control
Ensuring patient comfort is paramount during and after a surgical tooth extraction. The choice of anesthesia and the strategy for pain management are tailored to the complexity of the procedure and the individual patient’s needs and medical history.
- Local Anesthesia: This is the cornerstone of pain control during the extraction itself. A local anesthetic agent is injected into the tissues surrounding the tooth, blocking nerve impulses and rendering the area numb. Patients will feel pressure and movement but should not experience sharp pain.
- Sedation: For patients who experience anxiety or for more involved surgical extractions, various levels of sedation can be employed:
- Nitrous Oxide (Laughing Gas): A mild sedative inhaled through a mask, which helps patients relax and reduces anxiety. They remain conscious and able to respond to instructions.
- Oral Sedation: Medication taken by mouth before the appointment to induce a state of relaxation. The level of sedation can vary.
- Intravenous (IV) Sedation: A sedative is administered directly into a vein, producing a deeper state of relaxation or even a twilight sleep. The patient is closely monitored throughout the procedure.
- Post-Operative Pain Management: Once the local anesthetic wears off, some degree of pain and discomfort is expected. Pain management is typically achieved through a combination of:
- Over-the-Counter (OTC) Pain Relievers: Ibuprofen (Advil, Motrin) or acetaminophen (Tylenol) are often recommended for mild to moderate pain. NSAIDs like ibuprofen also help reduce swelling.
- Prescription Pain Medication: For more significant pain, a stronger pain reliever, often an opioid or a combination medication, may be prescribed for a limited time. These should be taken only as directed due to the risk of side effects and dependence.
- Ice Packs: Applying ice packs to the outside of the face over the surgical area can help reduce swelling and discomfort, particularly in the first 24-48 hours.
Effective communication with the dental professional about pain levels and adherence to the prescribed pain management regimen are crucial for a comfortable recovery.
6. Navigating Potential Challenges: Risks and Complications
While surgical tooth extractions are common procedures, like any surgery, they carry potential risks and complications. While relatively infrequent, it’s important for patients to be aware of them:
- Pain and Swelling: Expected to some degree, but excessive or prolonged pain and swelling could indicate an issue like infection or dry socket.
- Bleeding: Some oozing of blood from the socket is normal in the first 24 hours. Persistent or heavy bleeding requires immediate attention.
- Dry Socket (Alveolar Osteitis): This painful condition occurs when the blood clot that forms in the socket dislodges or dissolves prematurely, exposing the underlying bone and nerves. It is more common in surgical extractions, particularly of lower wisdom teeth, and is strongly associated with smoking.
- Infection: Although sterile techniques are used, infection is a possibility. Signs include increased pain, swelling, redness, warmth, and pus. Antibiotics may be prescribed preventatively or if an infection develops.
- Nerve Injury: The inferior alveolar nerve (which provides sensation to the lower lip, chin, and tongue) and the lingual nerve (which provides sensation and taste to the tongue) are located near the roots of lower teeth, especially wisdom teeth. In rare cases, these nerves can be bruised or damaged during extraction, leading to temporary or, very rarely, permanent numbness, tingling, or altered sensation.
- Damage to Adjacent Teeth: There is a small risk of damaging nearby teeth or their restorations during the extraction process.
- Sinus Perforation (Oroantral Communication): The roots of upper back teeth are often close to the maxillary sinuses. During extraction, an opening can occur between the tooth socket and the sinus. Small perforations often heal on their own, but larger ones may require surgical closure to prevent chronic sinus issues.
- Trismus (Difficulty Opening Mouth): Stiffness and soreness of the jaw muscles after surgery can make it difficult to open the mouth wide. This usually resolves within a week or two.
- Bruising: Discoloration of the skin around the jaw and neck can occur, particularly after more difficult extractions.
- Fracture of the Jawbone: Extremely rare, but a risk in complex extractions, especially if the jawbone is weakened.
Discussing these potential risks with your dental professional before the procedure is important, and following post-operative instructions carefully significantly reduces their likelihood.
7. The Road to Recovery: Post-Operative Care and Healing
Proper post-operative care is essential for a smooth recovery and to minimize the risk of complications after a D7610 procedure. The healing process takes time, and adherence to the dentist’s instructions is crucial.
Here are general guidelines for recovery:
- Bleeding Control: Bite firmly on the gauze pads placed over the extraction site for 30-60 minutes. Replace the gauze as needed. Some light oozing is normal for the first 24 hours. Avoid spitting or rinsing vigorously, as this can dislodge the blood clot.
- Pain Management: Take pain medication as prescribed or recommended by your dentist. It’s often best to take the first dose before the local anesthetic completely wears off.
- Swelling Reduction: Apply ice packs to the outside of the cheek over the surgical area for 20 minutes on, 20 minutes off, during the first 24-48 hours. Keeping your head elevated, even while sleeping, can also help reduce swelling.
- Rest: Plan to rest for the remainder of the day after surgery. Avoid strenuous activity for at least 24-48 hours, or longer if advised by your dentist.
- Diet: Stick to soft, cool foods and liquids immediately after surgery. Avoid hot foods and drinks, as well as using a straw, for the first 24-48 hours. Gradually reintroduce normal foods as tolerated, but avoid hard, crunchy, or sticky items that could irritate the extraction site for about a week.
- Oral Hygiene: Gently brush your teeth, avoiding the extraction site, the day after surgery. You may be advised to rinse gently with warm salt water (1/2 teaspoon of salt in a glass of warm water) several times a day after the first 24 hours to keep the area clean. Avoid commercial mouthwashes containing alcohol.
- Smoking and Alcohol: Absolutely avoid smoking and alcohol for at least 48 hours after surgery, as they significantly impede healing and increase the risk of dry socket.
- Follow-Up: Attend any scheduled follow-up appointments with your dentist or oral surgeon to ensure proper healing and remove sutures if necessary.
Healing time varies depending on the complexity of the extraction and individual factors. Initial healing of the gum tissue may take a couple of weeks, while bone remodeling and complete healing of the socket can take several months. Patience and diligent aftercare are key to a successful recovery.
8. Understanding the Investment: Billing, Insurance, and D7610
The cost of a D7610 dental procedure is typically higher than a simple extraction (D7140) due to the increased complexity, longer time involved, and often the need for specialized skills and equipment. Understanding the billing process and potential insurance coverage is important for patients.
- The Code D7610: As mentioned, this code specifically designates the surgical removal of a tooth requiring flap elevation and bone removal and/or tooth sectioning. This code communicates the complexity of the procedure to insurance providers.
- Factors Influencing Cost: The total cost can vary based on several factors:
- Complexity of the Extraction: An impacted wisdom tooth deeply embedded in bone will generally cost more to remove than a fractured tooth root requiring minimal bone removal.
- Location of the Tooth: Upper teeth might have different considerations than lower teeth.
- Type of Anesthesia/Sedation: Using IV sedation adds to the overall cost.
- Geographic Location: Dental fees vary by region.
- The Provider: Costs may differ between a general dentist performing the procedure and an oral surgeon (a specialist).
- Additional Procedures: If bone grafting is performed simultaneously, this will be billed separately (e.g., D7953 for placement of bone graft).
- Insurance Coverage: Dental insurance coverage for surgical extractions varies widely depending on the specific plan.
- Benefit Levels: Most insurance plans categorize procedures and cover them at different percentages. Surgical extractions are typically considered a “major” procedure and may be covered at a lower percentage (e.g., 50-80%) compared to basic procedures like fillings.
- Deductibles and Annual Maximums: Patients are usually responsible for meeting their plan’s deductible before insurance coverage kicks in. There is also often an annual maximum benefit amount that the insurance company will pay per year.
- Pre-Authorization: For D7610 procedures, particularly if performed by a specialist or involving impacted teeth, insurance companies often require pre-authorization. This involves submitting documentation (like X-rays and a treatment plan) to the insurer before the procedure to determine if it is covered and at what level. Obtaining pre-authorization is highly recommended to avoid unexpected out-of-pocket expenses.
- Medical vs. Dental Insurance: In some cases, particularly with impacted teeth or those involved in pathology, medical insurance might cover a portion of the cost, especially if the procedure is performed in a hospital or surgical center setting by an oral and maxillofacial surgeon. This is not always the case and depends on the specific medical plan and the reason for the extraction.
Patients should always contact their dental and/or medical insurance providers before a scheduled D7610 procedure to understand their specific coverage, co-pays, deductibles, and whether pre-authorization is required. Obtaining a detailed estimate from the dental office is also crucial for financial planning.
9. Simple vs. Surgical: D7140 vs. D7610
The distinction between a simple extraction (coded as D7140) and a surgical extraction (coded as D7610) is based on the complexity of the procedure, specifically the techniques required to remove the tooth. This difference has significant implications for both the clinical approach and the billing.
Here’s a table summarizing the key differences:
Essentially, if a tooth can be removed using only elevators and forceps without the need to cut the gum tissue, remove bone, or divide the tooth, it is likely a D7140. If any of these surgical steps are necessary, it falls under the category of D7610.
10. The Role of Technology in Modern Extractions
Technological advancements have significantly impacted the field of oral surgery, including D7610 procedures, enhancing precision, safety, and patient outcomes.
-
3D Imaging (Cone-Beam Computed Tomography – CBCT): CBCT provides detailed, three-dimensional images of the teeth, jawbones, and surrounding structures, including the location of nerves and sinuses. This advanced imaging allows for incredibly precise pre-operative planning, enabling the surgeon to visualize the tooth’s position, root anatomy, and relationship to vital structures, thereby minimizing risks during the procedure.
(Image Suggestion: A comparison image showing a traditional 2D dental X-ray next to a 3D CBCT scan of the same area.)
-
Piezosurgery: This technology uses ultrasonic vibrations to cut bone while minimizing trauma to soft tissues like nerves and blood vessels. It offers a higher level of precision for bone removal compared to traditional drills, which can be particularly beneficial in delicate areas or when working near nerves.
-
Advanced Surgical Instruments: Modern surgical instruments are designed for improved ergonomics, precision, and minimal invasiveness, contributing to smoother procedures and potentially faster healing.
-
Digital Workflow: Digital impressions and treatment planning software allow for virtual simulation of the extraction and precise planning of incisions and bone removal.
While not every D7610 procedure requires all of these technologies, their availability contributes to the increasing safety and predictability of complex tooth extractions.
11. The Importance of Comprehensive Care and Follow-Up
A successful D7610 procedure extends beyond the extraction itself. Comprehensive care involves thorough evaluation, meticulous planning, skilled execution, and diligent post-operative management.
- Pre-Operative Evaluation: A detailed medical history, dental history, clinical examination, and appropriate radiographs (including potentially a CBCT scan) are crucial for diagnosing the need for a surgical extraction and planning the procedure. This also allows for assessment of any underlying health conditions that might affect the surgery or recovery.
- Patient Education: Clearly explaining the procedure, the reasons for it, potential risks and benefits, and what to expect during and after the extraction is vital for informed consent and reducing patient anxiety.
- Skilled Provider: D7610 procedures require a higher level of surgical skill and experience. While some general dentists are trained in surgical extractions, complex cases, particularly impacted wisdom teeth or those close to vital structures, are often best managed by an oral and maxillofacial surgeon.
- Post-Operative Instructions: Providing clear, written, and verbal post-operative instructions is essential for guiding the patient through the recovery period and minimizing complications.
- Follow-Up Care: Scheduled follow-up appointments allow the dental professional to monitor healing, remove sutures if needed, address any concerns, and ensure the patient is recovering as expected.
Comprehensive care ensures that the entire process, from the initial diagnosis to full recovery, is managed effectively, leading to the best possible outcome for the patient.
12. Conclusion: Appreciating the Complexity
The D7610 dental code represents a significant procedure in oral surgery – the surgical removal of a tooth requiring the elevation of a mucoperiosteal flap and the removal of bone and/or sectioning of the tooth. It is a necessary intervention for teeth that cannot be removed simply, such as impacted teeth, those with complex roots, or those involved in pathology. The procedure involves careful planning, precise surgical techniques, and meticulous post-operative care to ensure a successful outcome and minimize complications. Understanding the nuances of D7610 helps patients appreciate the complexity involved and the importance of seeking care from skilled dental professionals.
13. Frequently Asked Questions (FAQs)
-
Q: What is the difference between D7140 and D7610? A: D7140 is for a simple extraction using only elevators and forceps. D7610 is for a surgical extraction requiring lifting the gum tissue (flap), removing bone, or cutting the tooth into pieces.
-
Q: Will I be asleep for a D7610 procedure? A: You will be numb with local anesthesia. Depending on the complexity and your anxiety level, sedation (like nitrous oxide, oral sedation, or IV sedation) may also be used. You will discuss anesthesia options with your dentist or surgeon.
-
Q: How long does recovery take after a D7610 extraction? A: Initial recovery with reduced pain and swelling typically takes about a week. Complete healing of the socket can take several months. Following post-operative instructions is crucial for a smooth recovery.
-
Q: What are the main risks of a D7610 procedure? A: Risks include pain, swelling, bleeding, dry socket, infection, nerve injury (rare), damage to adjacent teeth, and sinus perforation (for upper teeth). Your dental professional will discuss these risks with you.
-
Q: Is a D7610 procedure always done by an oral surgeon? A: While general dentists can perform some D7610 procedures, complex cases, especially impacted wisdom teeth, are often referred to oral and maxillofacial surgeons who have specialized training.
-
Q: Will my dental insurance cover a D7610 procedure? A: Coverage varies by plan. D7610 is usually considered a major procedure and may have different coverage levels than simple extractions. Pre-authorization is often required. Check with your insurance provider.
-
Q: Can I smoke after a D7610 extraction? A: No, smoking significantly increases the risk of dry socket and impedes healing. You should avoid smoking for at least 48 hours, or preferably longer, after the procedure.