The Ultimate Guide to Dental Codes for Resin Composite Restorations
Resin composite fillings have revolutionized modern dentistry, offering a tooth-colored alternative to traditional amalgam fillings. However, accurately billing for these procedures requires a deep understanding of Current Dental Terminology (CDT) codes. Misusing these codes can lead to claim denials, delayed payments, or even audits.
This comprehensive guide will explore every aspect of dental coding for resin composite restorations, including:
-
The most commonly used CDT codes
-
Differences between anterior and posterior composites
-
Insurance billing best practices
-
How to avoid coding errors
Whether you’re a dentist, dental assistant, or insurance biller, this article will help you navigate the complexities of resin composite coding with confidence.
2. Understanding Dental Billing Codes
Dental procedures are categorized using CDT codes, maintained by the American Dental Association (ADA). These codes standardize billing and ensure consistency across insurance claims.
Why Accurate Coding Matters
-
Ensures proper reimbursement
-
Reduces claim rejections
-
Prevents legal and compliance issues
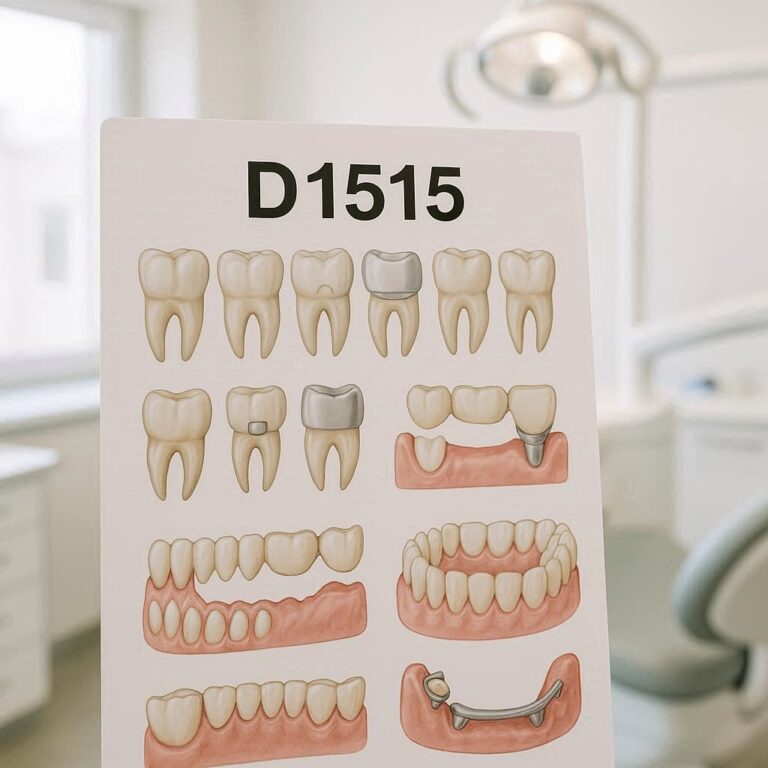
Types of Codes for Resin Composites
Resin composite restorations fall under “Direct Restorations” in the CDT manual. The codes vary based on:
-
Tooth location (anterior vs. posterior)
-
Number of surfaces restored
-
Material used
3. What is Resin Composite?
Resin composite is a tooth-colored filling material made of a mixture of plastic and fine glass or ceramic particles. It bonds directly to the tooth structure, providing both aesthetic and functional benefits.
Advantages Over Amalgam
✔ Aesthetic (matches natural teeth)
✔ Bonds chemically to tooth structure
✔ Requires less tooth preparation
✔ Free of mercury (unlike amalgam)
Disadvantages
✖ More technique-sensitive
✖ Higher cost
✖ May wear faster in high-stress areas
4. Common Dental Codes for Resin Composite Restorations
The most frequently used CDT codes for resin composites include:
Table 1: Resin Composite Restoration Codes
| CDT Code | Description | Typical Use Case |
|---|---|---|
| D2390 | Resin composite – 1 surface, anterior | Chipped front tooth |
| D2391 | Resin composite – 2 surfaces, anterior | Two-surface filling on incisor |
| D2392 | Resin composite – 3 surfaces, anterior | Large filling on canine |
| D2393 | Resin composite – 4+ surfaces, anterior | Extensive decay on front tooth |
| D2394 | Resin composite – 1 surface, posterior | Small cavity on molar |
| D2330 | Resin composite – 1 surface, anterior (alternative code) | Some insurers prefer this |
| D2331 | Resin composite – 2 surfaces, anterior | Alternative to D2391 |
| D2332 | Resin composite – 3 surfaces, anterior | Alternative to D2392 |
| D2335 | Resin composite – 4+ surfaces, anterior | Alternative to D2393 |
Key Differences Between Codes
-
D2390-D2394 are the most widely accepted codes.
-
D2330-D2335 are older codes still used by some insurers.
-
Always verify with the patient’s insurance which codes they recognize.
5. Differences Between Amalgam and Composite Codes
Amalgam fillings use a different set of codes (D2140-D2150). Billing a composite under an amalgam code can lead to denials or underpayment.
Why Insurance Companies Care
-
Composites are more expensive than amalgam.
-
Some plans only cover amalgam unless medically necessary.
When to Use a Composite Code vs. Amalgam
-
If the patient requests a tooth-colored filling → Use composite codes.
-
If the insurer only covers amalgam → Obtain pre-authorization for composite.
6. Insurance Considerations for Composite Fillings
Will Insurance Cover Composite Fillings?
✅ Yes, if:
-
The plan allows “tooth-colored fillings.”
-
The dentist documents medical necessity (e.g., allergies to amalgam).
❌ No, if:
-
The plan only covers amalgam.
-
The filling is purely cosmetic.
How to Increase Approval Chances
-
Submit pre-treatment estimates.
-
Include narrative notes explaining necessity.
-
Use accurate surface counts (single vs. multi-surface).
7. Step-by-Step Guide to Billing Resin Composite Procedures
Step 1: Verify Insurance Coverage
-
Check if the plan covers composites.
-
Determine if prior authorization is needed.
Step 2: Document the Procedure
-
Note the tooth number and surfaces involved.
-
Take pre-op and post-op photos if possible.
Step 3: Submit the Claim
-
Use the correct CDT code.
-
Attach supporting documentation if required.
Step 4: Follow Up on Denials
-
If denied, appeal with additional notes/X-rays.
8. Common Mistakes in Dental Coding for Composites
❌ Using amalgam codes for composites → Leads to underpayment.
❌ Miscounting surfaces → Can cause claim rejection.
❌ Not documenting medical necessity → Risk of denial.
How to Avoid Errors
✔ Double-check codes before submission.
✔ Train staff on updated CDT changes.
✔ Use dental billing software with built-in code validation.
9. How to Maximize Reimbursement for Composite Restorations
Tips for Higher Payouts:
-
Use the most specific code (e.g., D2394 instead of a generic code).
-
Submit X-rays to justify multi-surface fillings.
-
Appeal wrongful denials with additional evidence.

10. Frequently Asked Questions (FAQs)
Q1: Can I bill a composite filling as an amalgam to get it covered?
No. This is considered fraud. Always use the correct CDT code.
Q2: Why was my composite filling claim denied?
Possible reasons:
-
The plan only covers amalgam.
-
Incorrect surface count was reported.
-
Lack of medical necessity documentation.
Q3: What’s the difference between D2390 and D2330?
Both are for single-surface anterior composites, but some insurers prefer one over the other.
Q4: How do I know how many surfaces to bill?
Count each distinct tooth surface involved (e.g., mesial + occlusal = 2 surfaces).
11. Conclusion
Properly coding resin composite restorations ensures accurate reimbursement and compliance. Always use the latest CDT codes, document thoroughly, and verify insurance policies. By following these guidelines, dental practices can minimize denials and maximize revenue while providing high-quality patient care.