codes for dental benefits: Understanding CDT, HCPCS, and ICD-10 for Optimal Claims Processing
Dental benefit codes are the backbone of insurance claims processing, ensuring that dental practices receive timely and accurate reimbursements. With the increasing complexity of dental insurance policies, understanding CDT, HCPCS, and ICD-10 codes is more critical than ever.
Mistakes in coding can lead to claim denials, delayed payments, and even audits, costing dental practices thousands of dollars annually. This comprehensive guide will break down everything you need to know about dental benefit codes, including:
- The differences between CDT, HCPCS, and ICD-10 codes
- How to apply them correctly for maximum reimbursement
- Common coding errors and how to avoid them
By the end of this article, you’ll have a master-level understanding of dental coding, ensuring smoother claims processing and improved revenue cycle management.

2. Understanding Dental Benefit Codes
What Are Dental Benefit Codes?
Dental benefit codes are standardized alphanumeric identifiers used to describe dental procedures, diagnoses, and services for insurance billing. The three primary coding systems in dentistry are:
- CDT Codes – Maintained by the American Dental Association (ADA), these describe dental procedures.
- HCPCS Codes – Used for medical-dental crossover procedures (e.g., sleep apnea devices).
- ICD-10 Codes – Diagnostic codes that justify medical necessity.
Importance of Accurate Coding in Dentistry
- Ensures Proper Reimbursement – Incorrect codes lead to claim rejections.
- Prevents Fraud and Abuse – Upcoding or unbundling can trigger audits.
- Improves Patient Experience – Clear coding reduces billing disputes.
3. Types of Dental Coding Systems
CDT Codes (Current Dental Terminology)
The CDT Code set is updated annually by the ADA and includes five-character alphanumeric codes (e.g., D0120 for periodic oral evaluation).
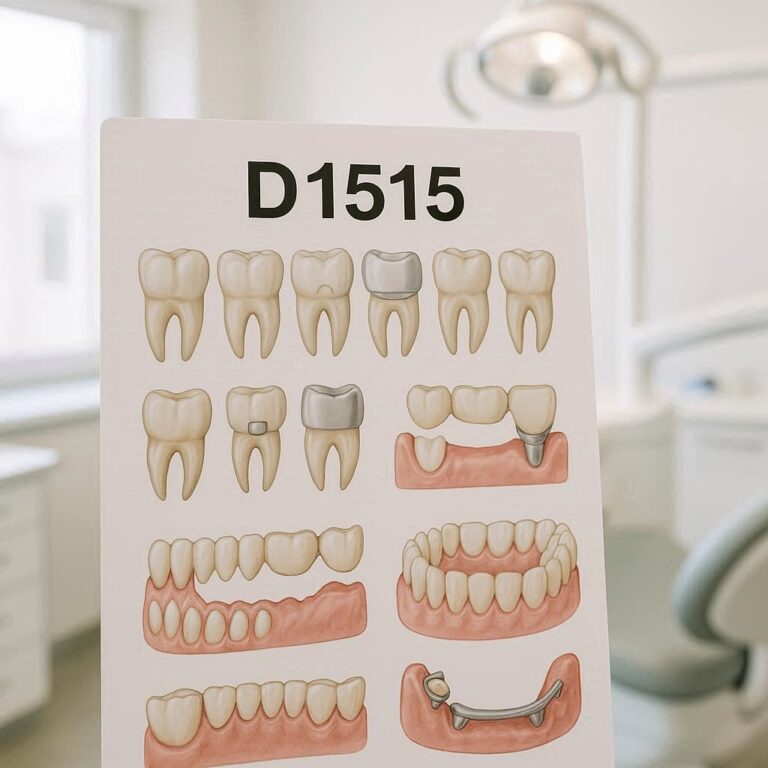
Categories of CDT Codes
| Category | Code Range | Description |
|---|---|---|
| Diagnostic | D0100-D0999 | Exams, X-rays |
| Preventive | D1000-D1999 | Cleanings, sealants |
| Restorative | D2000-D2999 | Fillings, crowns |
HCPCS Codes
HCPCS (Level II) codes are used when a dental procedure overlaps with medical billing, such as:
- Durable Medical Equipment (DME) – E0486 (Oral device for sleep apnea)
- Surgical Procedures – S8262 (Dental implant)
ICD-10-CM Codes
ICD-10 codes explain why a procedure was necessary (e.g., K02.9 for dental caries).
4. How Dental Benefit Codes Work
Role in Insurance Claims
- CDT = What was done?
- ICD-10 = Why was it done?
- HCPCS = Was it medically necessary?
Common Challenges in Dental Coding
- Frequency Limitations (e.g., only two cleanings per year covered)
- Medical Necessity Disputes (e.g., implants vs. dentures)
5. Key CDT Codes Every Dentist Should Know
Preventive Codes (D1000-D1999)
- D1110 – Adult prophylaxis
- D1206 – Fluoride varnish
Restorative Codes (D2000-D2999)
- D2391 – Resin-based composite filling (1 surface)
11. Conclusion
Dental benefit codes are essential for efficient claims processing, reducing denials, and maximizing reimbursements. By mastering CDT, HCPCS, and ICD-10 codes, dental practices can streamline billing, avoid compliance risks, and improve patient satisfaction. Stay updated with annual changes, document thoroughly, and train staff regularly to ensure coding accuracy.
12. Frequently Asked Questions (FAQs)
Q1: How often are CDT codes updated?
A: The ADA updates CDT codes annually (effective January 1).
Q2: Can I use both CDT and HCPCS codes on the same claim?
A: Yes, if the procedure has both dental and medical components (e.g., oral surgery).
Q3: What is the most common reason for dental claim denials?
A: Missing or incorrect ICD-10 codes (lack of medical necessity documentation).