Demystifying D0364 dental code: A Deep Dive into 3D Dental Imaging and Its Revolutionary Impact on Patient Care
For over a century, two-dimensional X-ray imaging has been the backbone of dental diagnosis. From humble bitewings to panoramic radiographs, these images have provided invaluable glimpses into the hidden structures of the oral cavity. However, they share a fundamental limitation: they flatten a complex, three-dimensional world into a two-dimensional picture. This compression of anatomy inevitably leads to superimposition of structures, distortion, and a lack of critical spatial information. How close is that lower wisdom tooth to the nerve? What is the exact width and density of the jawbone for an implant? Is that crack in the tooth propagating toward the root? With 2D imaging, dentists often had to make educated guesses or proceed with a degree of uncertainty.
The introduction of Cone Beam Computed Tomography (CBCT) marked a paradigm shift in dental diagnostics, and at the heart of this revolution is a specific code: D0364. This code represents more than just a procedure; it signifies the transition from guessing to knowing, from approximation to precision. It is the key that unlocks a detailed, interactive, three-dimensional map of a patient’s craniofacial anatomy, enabling a level of diagnosis and treatment planning previously confined to hospital-based medical CT scanners.
This article serves as the definitive guide to D0364 dental code. We will embark on a detailed exploration of this transformative technology, from its technical underpinnings and vast clinical applications to its practical implications for patients and practitioners. Our journey will demystify the code, illuminate its profound impact on modern dentistry, and glimpse into the future it is helping to shape.

2. What Exactly is Dental Code D0364? Decoding the Terminology
In the dental world, procedures are categorized and billed using Current Dental Terminology (CDT) codes, maintained by the American Dental Association (ADA). These codes ensure uniformity and clarity in communication between dental offices, patients, and insurance companies.
D0364 is the CDT code for Cone Beam CT – craniofacial data capture.
Let’s break down this official descriptor:
-
Cone Beam CT (CBCT): This is the specific technology. Unlike traditional medical CT scanners that use a fan-shaped beam that spirals around the patient, CBCT uses a cone-shaped X-ray beam that projects onto a rectangular, two-dimensional detector. This allows it to capture a large volume of data—essentially, the entire area of interest—in a single, rapid rotation (typically 10-40 seconds).
-
Craniofacial: This term specifies the anatomical region. “Craniofacial” refers to the skull (cranium) and face (facial). This distinguishes D0364 from other medical CT scans of the head, which might focus on the brain, and confirms its use for dental and maxillofacial structures, including the jaws, sinuses, nasal cavity, and temporomandibular joints (TMJs).
-
Data Capture: This is a crucial phrase. D0364 specifically refers to the acquisition of the raw volumetric data set. It is the act of performing the scan and capturing the millions of individual data points (voxels) that make up the 3D image. It is important to note that this code does not include the interpretation and report of the scan, which is billed under a separate code, D0366.
In essence, when a dentist charges for D0364, they are billing for the use of the expensive CBCT machine, the technician’s time to operate it, the proprietary software to reconstruct the data, and the secure storage of the large digital file.
3. The Technical Anatomy of a Cone Beam CT Scan: How It Works
Understanding the mechanics of a CBCT scan helps appreciate its value and limitations.
The Cone-Shaped Beam vs. Traditional Fan-Shaped CT
Traditional medical CT uses a narrow, fan-shaped beam that collects data slice-by-slice as the source and detector make multiple rotations around the patient. These individual slices are then computationally stacked to create a 3D volume. CBCT simplifies this mechanically. The X-ray source and a flat-panel detector are mounted on opposite sides of a rotating gantry. As they make one complete 360-degree (or slightly less) rotation around the patient’s head, the cone-shaped beam projects through the area of interest onto the detector, capturing hundreds of 2D “basis images” or projections from different angles.
The Image Acquisition Process: From Scan to 3D Model
-
Positioning: The patient is carefully positioned seated, standing, or lying down, depending on the machine. A head stabilizer or chin rest ensures minimal movement.
-
Scanning: The machine rotates around the patient’s head. During this rotation, the X-ray source pulses intermittently, and the detector captures a sequential series of 2D images.
-
Reconstruction: This is where the magic happens. The hundreds of acquired 2D images are sent to a computer workstation running specialized software. Using sophisticated algorithms known as Feldkamp, Davis, and Kress (FDK) reconstruction, the software back-projects the 2D data to compute and generate a 3D volumetric data set.
Understanding Voxels: The 3D Pixels of Data
A 2D digital image is made of pixels (picture elements). A 3D CBCT volume is made of voxels (volume elements). Each voxel is a tiny cube of data that is assigned a grayscale value based on the radiodensity of the tissue at that specific point. This volumetric grid of voxels is what allows the software to be manipulated and sliced in any plane—axial, coronal, sagittal—or to create 3D surface renderings of the bones and teeth. The size of these voxels determines the resolution of the scan; smaller voxels (e.g., 0.075mm – 0.2mm) yield higher resolution but often at the cost of increased radiation dose or a smaller field of view.
4. Clinical Applications: When and Why is D0364 Used?
CBCT is not a routine screening tool. It is a diagnostic modality used when its specific benefits are required to answer a clinical question that cannot be sufficiently addressed with 2D imaging. Its applications are vast and transformative across nearly every dental specialty.
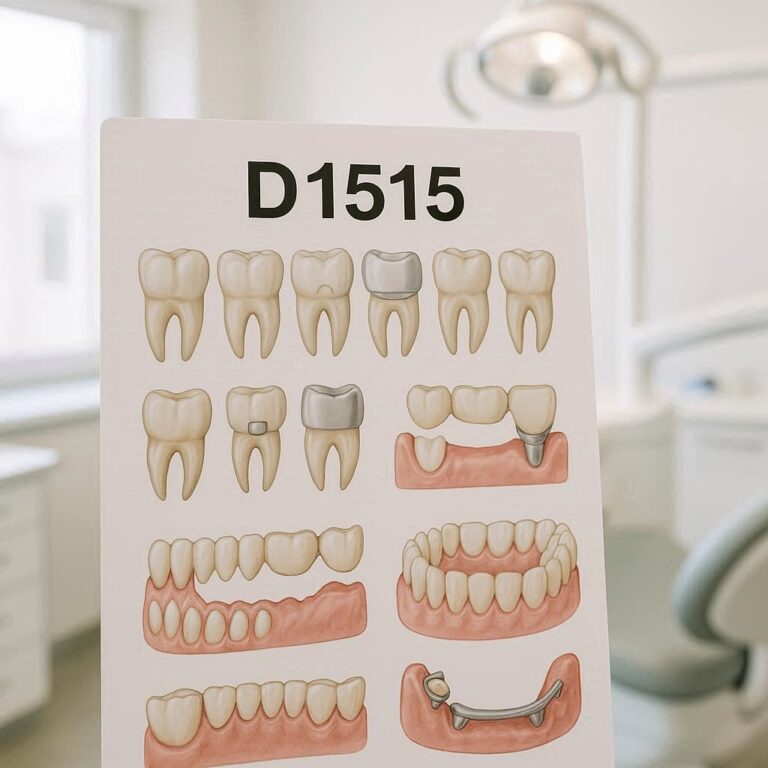
The Gold Standard for Dental Implant Planning
This is one of the most common and critical uses of D0364. CBCT provides exact information:
-
Bone Quantity and Quality: Precise measurement of bone height, width, and density at the proposed implant site.
-
Anatomical Guidance: Clear identification of vital structures to avoid, such as the inferior alveolar nerve canal, mental foramen, maxillary sinuses, and nasal cavity.
-
Virtual Surgery: The DICOM (Digital Imaging and Communications in Medicine) data from the CBCT scan can be imported into implant planning software. The surgeon can then virtually place the implant of the chosen size and brand in the ideal position, avoiding critical structures and ensuring optimal biomechanics.
-
Fabrication of Surgical Guides: The virtual plan can be used to 3D print a surgical guide—a stent that fits over the teeth or gums and guides the drill to the exact planned position, depth, and angle. This facilitates flapless, minimally invasive surgery, reducing patient recovery time and improving outcomes.
Endodontics: Seeing the Unseeable in Root Canals
For root canal treatment, CBCT is invaluable in complex cases:
-
Diagnosing Complex Root Anatomy: Identifying extra canals, curved canals, or complex morphologies (like C-shaped canals) that are missed on 2D films.
-
Detecting Apical Periodontitis: Identifying periapical lesions that are not visible on periapical radiographs, especially in areas with thick buccal or lingual cortical plates.
-
Managing Endodontic Failures: Differentiating between a failed healing and a surgical complication, identifying missed canals, locating separated instruments, and diagnosing vertical root fractures (though beam hardening artifacts from root canal fillings can complicate this).
-
Traumatic Dental Injuries: Assessing the true extent of root fractures, luxations, and alveolar fractures.
Oral Surgery: Navigating Complex Extractions and Pathologies
-
Impacted Teeth: Precisely localizing impacted teeth (especially third molars) in all three dimensions, determining their relationship to the inferior alveolar nerve, and planning the most conservative access for removal.
-
Pathology Assessment: Evaluating the size, extent, and internal structure of cysts, tumors, and other lesions of the jaws. CBCT provides superior detail of the bony margins and effects on surrounding anatomy compared to 2D imaging.
-
Orthognathic Surgery: Planning for corrective jaw surgery requires detailed 3D models of the skeletal relationship. CBCT data is used for virtual surgical planning (VSP), where the surgeon performs the osteotomies and moves the jaw segments on the computer before the actual surgery, often leading to the fabrication of custom guides and splints.
Orthodontics: Precision Planning for Aligned Smiles
-
Impacted Canines: Precisely locating ectopically erupting or impacted canine teeth and assessing their effect on adjacent tooth roots.
-
Airway Analysis: Evaluating the nasal airway and pharyngeal space, which can be a factor in sleep-disordered breathing and craniofacial development.
-
Bone Assessment: Evaluating root angulation and proximity to cortical bone plates, which is critical for planning orthodontic tooth movement and minimizing the risk of root resorption.
-
Cephalometric Analysis: 3D CBCT cephalometry offers significant advantages over traditional 2D lateral cephalograms by eliminating magnification, distortion, and superimposition errors.
Temporomandibular Joint (TMJ) Analysis
CBCT provides high-resolution, sub-millimeter images of the bony components of the TMJ. It is the imaging modality of choice for evaluating:
-
Osteoarthritis (erosions, osteophytes, sclerosis)
-
Condylar position and morphology
-
Ankylosis
-
Fractures
Periodontics: Assessing Bone Loss in Three Dimensions
While traditional radiographs show the height of bone loss, CBCT reveals the ** morphology** of the defect—its width, depth, and configuration (e.g., craters, furcation involvements, dehiscences, fenestrations). This 3D information is critical for predicting prognosis and planning advanced regenerative surgical procedures.
Airway Analysis and Sleep Apnea Diagnosis
A large-field-of-view CBCT scan can capture the entire upper airway, from the nasal passages to the hypopharynx. Software can calculate the cross-sectional area and volume of the airway, which is valuable data for oral and maxillofacial surgeons, orthodontists, and sleep physicians in diagnosing obstructive sleep apnea (OSA) and planning treatments like maxillomandibular advancement surgery.
5. The Patient Experience: What to Expect During a CBCT Scan
For a patient, a CBCT scan is a straightforward and relatively quick procedure, often less intimidating than a traditional medical CT scan due to the open design of most units.
Pre-Scan Preparation
-
Justification: The dentist will explain why the CBCT scan is necessary for their specific case, ensuring the benefits outweigh the risks.
-
Medical History: A review of the patient’s medical and dental history is conducted.
-
Pregnancy Screening: It is standard protocol to ask female patients of childbearing age if there is any chance they could be pregnant. Elective X-ray imaging is generally avoided during pregnancy.
-
Removing Artifacts: The patient will be asked to remove any metal objects that could interfere with the image, such as glasses, jewelry, hairpins, hearing aids, and, if possible, removable dental appliances like partial dentures.
The Scanning Procedure Step-by-Step
-
The patient is positioned in the center of the machine, typically seated or standing.
-
A positioning apparatus (e.g., a chin rest and head stabilizers) is adjusted to align the patient’s head correctly. The technician will give clear instructions to remain perfectly still during the scan, as movement creates blurring artifacts.
-
The technician steps out of the room to the control console.
-
The rotating gantry, which contains the X-ray source and detector, will make a single, slow rotation around the patient’s head. The machine may emit a soft humming or buzzing sound during this process, which usually lasts between 10 and 40 seconds.
-
Once the rotation is complete, the scan is over. The entire appointment, from positioning to completion, often takes less than 10 minutes.
Post-Scan: Analysis and Interpretation
The raw data is reconstructed by the software. The dentist—or in many cases, a oral and maxillofacial radiologist—will then analyze the 3D dataset on a computer monitor. They will scroll through the axial, coronal, and sagittal slices, create panoramic reconstructions, and generate 3D renderings to make a diagnosis and create a detailed report. This interpretation is a separate procedure (D0366) from the capture of the data (D0364).
6. D0364 vs. D0366, D0367, D0368: Navigating the Family of 3D Codes
D0364 is part of a family of codes. Understanding the differences is crucial for accurate billing and communication.
-
D0364 – Cone beam CT – craniofacial data capture: The acquisition of the 3D volumetric dataset.
-
D0366 – Cone beam CT – interpretation and report: The professional service of analyzing the captured data, formulating a diagnosis, and generating a written report. This is often performed by a specialist.
-
D0367 – Cone beam CT – limited field of view: A data capture code for a scan of a small, focused area (e.g., a few teeth and their immediate surroundings).
-
D0368 – Cone beam CT – large field of view: A data capture code for a scan of one or both jaws, including the TMJs and sinuses.
The primary differentiator between D0364, D0367, and D0368 is the Field of View (FOV). FOV is the maximum diameter and height of the cylindrical or spherical volume of tissue that is captured during the scan. It is selected by the clinician based on the diagnostic need.
Comparison of Common CBCT CDT Codes
| CDT Code | Procedure Name | Description | Typical Field of View (FOV) | Common Use Cases |
|---|---|---|---|---|
| D0364 | Cone beam CT – craniofacial data capture | General code for capturing a 3D dataset. | Varies by machine and selection. Serves as a default when a more specific code isn’t used. | A wide range of applications. |
| D0367 | Cone beam CT – limited field of view | Capture of a small, focused 3D dataset. | Typically < 10 cm in diameter, capturing a small region (e.g., a quadrant of teeth). | Single implant site assessment, endodontic evaluation of a specific tooth, localized pathology. |
| D0368 | Cone beam CT – large field of view | Capture of an extensive 3D dataset. | Typically > 10 cm in diameter, capturing one or both full arches, sinuses, TMJs. | Orthodontic planning, multiple implant planning, orthognathic surgery planning, airway analysis. |
| D0366 | Cone beam CT – interpretation and report | The professional service of analyzing the data and writing a diagnostic report. | N/A (applies to any captured dataset). | Always reported in addition to a data capture code (D0364, D0367, D0368) when performed by a different provider. |
Choosing the Right Code: Field of View (FOV) is Key
The principle of ALARA (As Low As Reasonably Achievable) applies not just to dose but also to the area irradiated. A dentist should always choose the smallest FOV that will answer the clinical question. There is no need to scan an entire jaw to look at one tooth. Therefore, for a single implant site, D0367 would be the most appropriate and conservative code. For planning treatment for a full arch of implants, D0368 would be necessary. D0364 remains a valid, broader code used by many practices.
7. The Benefits and Advantages of CBCT Imaging
The adoption of CBCT is driven by its profound advantages over traditional 2D imaging.
Unparalleled Diagnostic Accuracy
CBCT eliminates the superimposition, distortion, and magnification inherent in 2D radiography. It provides an undistorted, true-scale, three-dimensional view of the area of interest, drastically reducing diagnostic uncertainty and the potential for clinical surprises.
Enhanced Patient Safety and Reduced Radiation Exposure
While CBCT delivers a higher radiation dose than a single intraoral X-ray, it delivers a significantly lower dose than a traditional medical CT scan of the same region—often by an order of magnitude (10-20 times less). This makes high-resolution 3D imaging accessible in the dental office with a much more favorable risk-benefit profile.
Improved Patient Communication and Case Acceptance
A 3D color-rendered model of a patient’s own anatomy is an incredibly powerful communication tool. Dentists can rotate the model, zoom in on problem areas, and visually explain the diagnosis and proposed treatment plan. This visual evidence dramatically improves patient understanding, trust, and acceptance of often complex and expensive treatments like implants and surgery.
Facilitating Minimally Invasive Procedures
As mentioned with guided implant surgery, the precision of CBCT allows for procedures that are less invasive, with smaller flaps or even no flaps at all. This translates to less postoperative pain, reduced swelling, and faster healing times for the patient.
8. Addressing the Concerns: Risks, Limitations, and Safety
Despite its benefits, CBCT is not without its drawbacks, which must be carefully managed.
Radiation Dose: Putting It in Perspective
Radiation exposure from dental CBCT is not zero, and it must be justified. However, context is vital. The effective dose from a small FOV CBCT scan can be comparable to a few days of natural background radiation or equivalent to a panoramic X-ray plus a small series of intraoral films. A large FOV scan might be equivalent to a cross-country flight. Dentists are trained to weigh this small risk against the significant diagnostic benefit for the individual patient.
The ALARA Principle (As Low As Reasonably Achievable)
This is the guiding principle of radiology. Every CBCT scan must be:
-
Justified: There must be a clear clinical need that cannot be met with a lower-dose alternative.
-
Optimized: The scan parameters (kVp, mA, FOV, voxel size, scan time) must be set to use the lowest possible dose that will still yield a diagnostically acceptable image.
Artifacts and Image Quality Limitations
CBCT images can be degraded by artifacts, which are distortions or errors in the image not present in the actual object. Common artifacts include:
-
Beam Hardening: Causes streaks and dark bands, often seen around dense metallic restorations (amalgam, crowns) or implants.
-
Scatter: Reduces image contrast.
-
Motion Artifact: Blurring caused by patient movement during the scan.
These artifacts can sometimes mimic pathology or obscure critical anatomical details.
The Importance of Proper Training and Interpretation
A 3D dataset is far more complex than a 2D image. Interpreting it requires extensive training in craniofacial anatomy and radiology. Misinterpretation can lead to misdiagnosis. Many general dentists who own CBCT machines will often send their scans to oral and maxillofacial radiologists for expert interpretation (coded as D0366) to ensure accuracy.
9. The Financial Aspect: Cost, Insurance, and Reimbursement for D0364
The financial considerations of CBCT are multifaceted.
Understanding the Cost Structure
The cost of a CBCT scan for a patient can range from $200 to $500+ depending on:
-
Geographic location of the practice.
-
Type of scan (FOV): A large FOV (D0368) is typically more expensive than a limited FOV (D0367).
-
Whether interpretation (D0366) is included or performed by a third-party radiologist.
This cost reflects the high capital investment in the machine (often $70,000 – $150,000), ongoing maintenance costs, software licensing fees, and data storage requirements.
Navigating Dental Insurance Coverage
Insurance coverage for CBCT is improving but remains variable. Many insurers now cover CBCT for specific, well-justified procedures like implant planning and complex surgical extractions. However, they may deny it for more general diagnostic screening. Pre-authorization is often recommended. The patient’s out-of-pocket cost will depend on their plan’s coverage for “diagnostic imaging” or “special tests.”
Coding and Documentation Best Practices for Dentists
For a claim to be accepted, documentation is key. The patient’s record must clearly indicate:
-
The clinical justification for the scan (e.g., “CBCT ordered for precise localization of tooth #17 in relation to the inferior alveolar nerve canal prior to surgical extraction.”).
-
The specific CDT code used (D0364, D0367, or D0368).
-
A copy of the radiologist’s report (if D0366 was used).
Proper documentation demonstrates medical necessity and is critical for avoiding claim denials and audits.
10. The Future of CBCT and 3D Imaging in Dentistry
The technology is not standing still. The future of CBCT is focused on smarter, safer, and more integrated imaging.
Artificial Intelligence (AI) Integration and Automated Diagnostics
AI algorithms are being trained to read CBCT scans to perform tasks such as:
-
Automated Cephalometric Tracing: Instantly generating cephalometric analyses for orthodontics.
-
Pathology Detection: Flagging potential areas of concern like periapical lesions, osteopenia, or sinusitis.
-
Anatomical Landmarking: Automatically identifying key structures like nerves and foramina for implant planning.
AI will act as a powerful assistant to clinicians, improving consistency and efficiency in diagnosis.
3D Printing and Guided Surgery
The synergy between CBCT and 3D printing will only deepen. The digital plans created from CBCT data will continue to drive the production of not just surgical guides, but also custom implants, prosthetic frameworks, and anatomical models for pre-surgical simulation, making personalized medicine a standard in dentistry.
The Evolution of Low-Dose, High-Resolution Scanners
Ongoing hardware and software innovations are focused on further reducing radiation doses without sacrificing image quality. Techniques like iterative reconstruction algorithms can produce clear images from noisier, low-dose raw data. The goal is to make the already favorable risk-benefit profile of CBCT even better.
11. Conclusion: Integrating 3D Vision into Standard of Care
The D0364 code represents a fundamental shift in dental diagnostics, moving the profession from inferential 2D analysis to precise 3D visualization. While it requires careful justification, proper training, and an understanding of its limitations, Cone Beam CT has unequivocally elevated the standard of care in countless clinical scenarios. It empowers clinicians with unparalleled diagnostic confidence, enables minimally invasive and highly predictable treatments, and fosters transparent communication with patients. As technology continues to advance, making CBCT smarter and safer, its role as an indispensable tool in modern, evidence-based dentistry will only continue to grow.
12. Frequently Asked Questions (FAQs)
Q1: Is a CBCT scan painful?
A: No, the scan itself is completely painless and non-invasive. You simply need to remain still for a short period of time.
Q2: How much radiation am I exposed to from a dental CBCT?
A: The dose varies significantly based on the machine settings and the size of the area scanned. However, a typical small-FOV dental CBCT scan has an effective dose that is often comparable to a panoramic X-ray plus a few bitewing X-rays, and is vastly lower than a medical CT scan. Your dentist will always follow the ALARA principle to minimize your exposure.
Q3: Why did my dentist recommend a CBCT scan for my implant? Can’t they use a normal X-ray?
A: A traditional 2D X-ray cannot show the width of your bone or the precise spatial relationship between the proposed implant site and vital nerves and sinuses. CBCT provides a 3D map that is essential for planning a safe, predictable, and successful implant procedure, helping to avoid potential complications.
Q4: My insurance denied the claim for my CBCT scan. Why?
A: Insurance denials can occur if the insurance company determines the scan was not “medically necessary” based on their specific criteria. This is why pre-authorization is valuable and why your dentist’s documentation of the clinical justification is critical. Your dental office can appeal the denial with this supporting documentation.
Q5: How long does it take to get the results?
A: The 3D images are available almost immediately after the scan. However, if the images are being sent to a specialist for a formal interpretation and report (D0366), it may take a few days to receive the final written report. Your dentist will discuss the findings with you as soon as they are available.
13. Additional Resources
-
American Dental Association (ADA): The official source for Current Dental Terminology (CDT) codes and policy statements on the use of CBCT.
-
American Academy of Oral and Maxillofacial Radiology (AAOMR): The leading professional organization for experts in dental radiology. They provide clinical recommendations, guidelines, and position statements on the use of CBCT.
-
Food and Drug Administration (FDA) – White Paper: Cone-Beam Computed Tomography for Dental and Maxillofacial Radiology: A resource for understanding the safety and regulatory aspects of CBCT devices.
-
Image Gently Alliance: A coalition dedicated to promoting safe and effective use of medical imaging in children. They have specific guidelines for imaging in pediatric dentistry.