The Complete Guide to Dental Bone Graft Costs and Modern Alternatives
Imagine deciding to build your dream home. You’ve chosen the perfect design, the finest materials, and the most skilled architect. But there’s a problem: the land you want to build on is unstable, eroded, and simply cannot support the weight of the structure. No matter how beautiful the house, without a solid foundation, it is destined to fail.
This analogy perfectly encapsulates the critical relationship between your teeth and your jawbone. For millions of patients seeking to replace missing teeth with dental implants—the modern gold standard—the journey often begins not with the implant itself, but with assessing the landscape of the jaw. Years of tooth loss, periodontal disease, or trauma can lead to significant bone loss, creating a situation where there is simply not enough bone to anchor an implant. This is where the remarkable science of dental bone grafting comes in.
The decision to undergo a bone graft procedure is often accompanied by a swirl of questions, concerns, and, most prominently, confusion about cost. The price quotes can be startlingly varied and opaque. Is a $500 graft sufficient? Why might another be quoted at $3,000? What are you actually paying for? Furthermore, are there alternatives to this seemingly complex and expensive surgery?
This definitive guide is designed to be your comprehensive resource. We will demystify the entire process, from the cellular biology of bone regeneration to the intricate factors that determine the final cost. We will explore all available graft materials, detail the surgical procedure, and honestly examine the pros and cons of every potential alternative. Our goal is to empower you with the knowledge you need to have informed, productive conversations with your oral surgeon and to make the best decision for your oral health and financial well-being. Your journey to a restored smile starts with understanding the foundation.
2. Why Your Jawbone Matters: The Science of Bone Resorption
To appreciate the value of a bone graft, one must first understand the dynamic, living nature of the jawbone. It is not a static, rock-like structure but a highly active tissue that constantly remodels itself in response to stimulus.
The Tooth-Bone Connection
The jawbone’s primary purpose is to support teeth. The roots of your teeth are embedded in the jawbone, and every time you chew and bite, the force is transferred through the root into the surrounding bone. This pressure acts as a crucial stimulant, signaling to the body that the bone is needed and encouraging it to maintain its density and volume. It’s a classic case of “use it or lose it.”
The Consequences of Tooth Loss
When a tooth is lost, this natural stimulation ceases entirely. The body, in its efficient wisdom, perceives that the bone in that area is no longer necessary for support. It begins a process called resorption, where specialized cells called osteoclasts break down the bone matrix and reabsorb the minerals back into the body. This isn’t a minor change; studies show that the jawbone can lose 25-30% of its width in the first year after tooth extraction, and this resorption continues at a slower pace for the rest of a person’s life.
The loss is not just horizontal (width) but also vertical (height). Over time, this can lead to a significant collapse of the alveolar ridge—the part of the jaw that holds the teeth. This has functional and aesthetic consequences:
-
Collapsed Facial Appearance: The jaw supports the muscles and skin of the lower face. Severe bone loss can lead to a sunken look, thinning lips, a more pointed chin, and increased wrinkles around the mouth, making a person appear significantly older.
-
Compromised Function: Difficulty chewing and speaking can occur.
-
Shifting of Adjacent Teeth: The teeth next to the gap can tilt into the space, disrupting your bite.
-
Inability to Place Implants: This is the most direct issue for restorative dentistry. A standard dental implant typically requires about 1mm of bone around its circumference for stability. Inadequate bone volume dooms an implant to failure from the start.
Common Causes of Jawbone Deterioration
-
Tooth Extraction: The most common cause.
-
Periodontal (Gum) Disease: Advanced periodontitis is an infection that destroys the gum tissue and the bone that supports the teeth.
-
Dentures: Long-term wear of conventional dentures can accelerate bone loss as they often rest directly on the gums, providing no stimulatory effect to the underlying bone and can even compress it.
-
Trauma: An injury to the face or teeth can damage the bone.
-
Misalignment: A tooth that never erupts properly can fail to provide the necessary stimulus.
-
Medical Conditions: Osteoporosis and other systemic health issues that affect bone density.
3. What is a Dental Bone Graft? The Architect’s Blueprint
A dental bone graft is a surgical procedure that aims to rebuild and regenerate lost jawbone. Contrary to what the name might imply, the graft material itself is often not the final bone. Instead, think of it as a scaffolding or a framework.
The core principle is Guided Tissue Regeneration (GTR). The surgeon places the graft material in the area of deficiency. This material serves a dual purpose:
-
Osteoconduction: It acts as a physical scaffold that your body’s own cells can migrate across, like a trellis for a vine.
-
Osteoinduction: It encourages your body’s undifferentiated stem cells and osteoprogenitor cells to become bone-forming cells (osteoblasts).
The graft material slowly resorbs over a healing period of 4 to 9 months. As it resorbs, your body replaces it with its own, new, healthy, and vascularized bone—a process called osseointegration for the graft site. Once healed, this newly regenerated bone provides the necessary volume and density to securely place a dental implant.
The Ultimate Goal: Successful Dental Implants
While bone grafts can be performed for other reasons (to support a denture or correct a defect), their primary purpose in modern dentistry is to create a stable foundation for dental implants. An implant placed in sufficient, healthy bone has a success rate exceeding 95% over a 10-year period. The graft is the critical first investment in ensuring that long-term success.
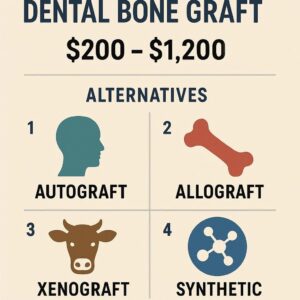
4. A Deep Dive into Dental Bone Graft Materials: Choosing the Right Building Blocks
The choice of graft material is one of the most significant factors influencing both the outcome and the cost of the procedure. Each type has distinct advantages, disadvantages, and ideal use cases.
Autografts (Your Own Bone) – The Gold Standard
An autograft involves harvesting bone from one part of a patient’s own body and transplanting it to the jaw.
-
Source: Common harvest sites include the chin (mandibular symphysis), the ramus (back of the jaw), the hip (iliac crest), or the tibia (shin bone).
-
Advantages:
-
Biocompatibility: Zero risk of disease transmission or immune rejection because it is your own tissue.
-
Viability: Contains living cells and natural growth factors, making it osteogenic (it can form new bone itself, not just guide it). This often leads to the fastest and most predictable healing.
-
-
Disadvantages:
-
Requires a Second Surgical Site: This means additional pain, potential complications, and longer surgery and recovery time.
-
Limited Supply: There is only so much bone that can be safely harvested from a patient.
-
-
Best For: Large defects where the highest predictability and volume of new bone formation are required.
Allografts (Human Donor Bone) – The Common Compromise
Allograft bone is sourced from a deceased human donor, processed by a tissue bank to ensure safety, and made available to surgeons.
-
Processing: The bone is rigorously tested for pathogens, freeze-dried, and demineralized (DFDBA) or processed in a way that removes all organic and cellular material, leaving only the mineral matrix.
-
Advantages:
-
No Second Surgery: Eliminates the pain and morbidity of a harvest site.
-
Good Availability: Comes in various forms (chips, blocks, powders) to suit different defects.
-
Osteoinductive Properties: Demineralized bone matrix retains bone morphogenetic proteins (BMPs) that can stimulate new bone growth.
-
-
Disadvantages:
-
The “Ick” Factor: Some patients are psychologically uncomfortable with using donor human tissue.
-
Theoretical Risk: While the processing is extremely effective, a minute theoretical risk of disease transmission exists.
-
-
Best For: The most common type of graft used in dentistry, suitable for a wide range of socket preservation and ridge augmentation procedures.
Xenografts (Animal-Derived Bone) – The Natural Scaffold
Xenografts are derived from another species, most commonly bovine (cow) or porcine (pig).
-
Processing: The animal bone is processed at extremely high temperatures to remove all organic material, leaving behind a sterile, biocompatible, calcium-phosphate scaffold that is very similar in structure to human bone.
-
Advantages:
-
Excellent space-maintaining properties; it resorbs very slowly, acting as a strong scaffold for a long time.
-
Abundant supply.
-
No human donor concerns.
-
-
Disadvantages:
-
Very slow resorption rate; it may remain in the site for years, meaning the new bone is a combination of your bone and the graft material.
-
Not osteoinductive on its own; it relies entirely on the body’s healing response.
-
-
Best For: Sinus lift procedures and large augmentations where a long-lasting scaffold is beneficial.
Alloplasts (Synthetic Bone) – The Technological Innovation
Alloplasts are completely laboratory-made, synthetic bone substitute materials.
-
Materials: Include hydroxyapatite (a natural bone mineral), tricalcium phosphate (TCP), bioactive glass, and polymer compounds.
-
Advantages:
-
Zero risk of disease transmission: from animal or human sources.
-
Highly consistent and predictable.
-
Can be engineered to have specific resorption rates.
-
Often more cost-effective than other options.
-
-
Disadvantages:
-
Variability in performance between different brands and formulas.
-
Generally considered less potent than autografts or allografts for large defects.
-
-
Best For: Small to medium defects, socket preservation, and as a filler material around other graft types.
Growth Factors: The Future is Now (PRF, PRP, BMP-2)
Modern grafting often involves enhancing the chosen material with growth factors to supercharge the healing process.
-
PRP (Platelet-Rich Plasma): A sample of the patient’s blood is centrifuged to concentrate the platelets. This concentrate, rich in growth factors, is mixed with the graft material to accelerate healing.
-
PRF (Platelet-Rich Fibrin): A second-generation, more advanced version of PRP. It creates a fibrin membrane that not only releases growth factors more slowly but also acts as a healing membrane itself.
-
BMP-2 (Bone Morphogenetic Protein-2): A powerful synthetic protein that directly stimulates the body to form new bone. It is very effective but also expensive and used typically for the most complex cases.
5. The Dental Bone Graft Procedure: A Step-by-Step Journey
Understanding the procedure can alleviate much of the anxiety surrounding it. It is typically performed under local anesthesia, often with IV sedation for patient comfort.
1. Initial Consultation and 3D Imaging:
The journey begins with a comprehensive exam. A CBCT (Cone Beam Computed Tomography) scan is indispensable. This 3D image allows the surgeon to precisely measure the bone’s height, width, and density and to identify critical structures like nerves and sinuses. It is the map that guides the entire procedure.
2. The Day of Surgery: What to Expect
-
Anesthesia: Administered for complete comfort.
-
Incision: The surgeon makes a small incision in the gum tissue to expose the underlying bone defect.
-
Preparation: The area is cleaned and prepared.
-
Graft Placement: The chosen graft material is packed into the defect. It is often covered with a collagen membrane to protect the graft and prevent soft tissue from growing into the space, allowing bone cells the time they need to regenerate.
-
Closure: The gum tissue is sutured closed. The goal is for the site to heal without infection and for the graft to integrate successfully.
3. The Healing Process: Osseointegration and Guided Tissue Regeneration
Healing is a multi-stage process:
-
First 2 Weeks: Focus on soft tissue healing. Patients must follow a soft diet, avoid disturbing the site, and practice meticulous oral hygiene as directed.
-
Months 1-4: Beneath the gum, the graft is being vascularized (new blood vessels grow into it) and is slowly being replaced by the patient’s own bone.
-
Months 4-9+: The bone matures and gains strength. The surgeon will take another CBCT scan to confirm the graft was successful and that there is now enough strong bone to proceed with the implant placement.
6. Decoding the Cost: A Comprehensive Breakdown of Dental Bone Graft Prices
The cost of a dental bone graft is not a single flat fee. It is a sum of multiple components, which explains the wide variation in quotes.
Factor 1: The Type and Quantity of Graft Material
This is a major cost driver. A few ccs of synthetic graft will be less expensive than a large volume of human donor block graft, which in turn is less expensive than the added cost and time of harvesting an autograft.
Factor 2: The Complexity and Scope of the Procedure
-
Socket Preservation: A simple graft placed immediately after an extraction to prevent collapse. This is the least expensive type.
-
Ridge Augmentation: rebuilding lost width and/or height of the jawbone. More complex and costly.
-
Sinus Lift: A specialized procedure to add bone to the upper jaw by lifting the sinus membrane. This is one of the most complex and expensive graft surgeries.
Factor 3: Geographic Location and Practice Overhead
A procedure in a major metropolitan area will almost always cost more than in a rural town due to higher rents, staff salaries, and general cost of living.
Factor 4: The Surgeon’s Expertise and Credentials
An experienced oral surgeon or periodontist who specializes in complex restorative cases will command higher fees than a general dentist. Their expertise, however, greatly reduces the risk of graft failure and complications.
Factor 5: Anesthesia and Surgical Facility Fees
If IV sedation or general anesthesia is used, an anesthesiologist’s fee will be added. Procedures performed in a hospital outpatient setting will be more expensive than those in a well-equipped dental office.
A Realistic Price Range Table
| Type of Bone Graft Procedure | Description | Typical Cost Range (Per Site) | Key Cost Determinants |
|---|---|---|---|
| Socket Preservation | Graft placed in an empty tooth socket immediately after extraction to prevent bone loss. | $300 – $600 | Type of graft material used, single vs. multi-rooted tooth. |
| Minor Ridge Augmentation | Adding bone to a small area of deficiency to prepare for a single implant. | $600 – $1,200 | Size of the defect, type of graft material, use of a membrane. |
| Major Ridge Augmentation | Rebuilding a significant portion of the jawbone, often using a block graft. | $1,500 – $3,500+ | Complexity, need for autograft, size of membrane required, operating time. |
| Sinus Lift (Lateral Window) | Adding bone to the upper jaw by lifting the sinus membrane. | $1,500 – $3,500+ | Surgeon’s fee, volume of graft material needed, anesthesia type. |
| Sinus Lift (Osteotome) | A less invasive “closed” sinus lift for smaller amounts of bone addition. | $1,000 – $2,500 | Suitability for the case, graft material. |
| Autograft Harvesting | Additional fee for harvesting the patient’s own bone. | $500 – $1,500+ | Harvest site (chin vs. hip), operating time. |
*Note: These costs are for the graft procedure only and do not include the subsequent cost of the dental implant and crown, which can add $2,000 – $5,000+ per tooth.*
7. Navigating Insurance and Financing Your Procedure
Unfortunately, dental insurance often provides limited coverage for bone grafts.
-
Dental Insurance: Most plans have an annual maximum ($1,000 – $1,500 is common). They may cover a portion of a graft if it is deemed “medically necessary” for the placement of an implant, but implants themselves are often not fully covered. You must check your specific plan’s exclusions.
-
Medical Insurance: In cases where bone loss is due to trauma or a medical condition (like cancer surgery), there is a higher chance of medical insurance covering part of the procedure. This requires careful documentation and coding by your surgeon’s office.
-
Financing: Most dental practices offer third-party financing through companies like CareCredit or LendingClub. These offer low- or no-interest payment plans for qualified applicants, making the cost much more manageable over time.
8. Exploring the Alternatives: Is a Graft Always Necessary?
For some patients, a traditional bone graft may not be the only path to an implant-supported tooth. Several alternatives exist, though they are highly case-specific.
Mini Dental Implants (MDIs)
These are implants with a smaller diameter (less than 3mm) than traditional implants.
-
How they avoid grafting: They require less bone volume for placement.
-
Pros: Less invasive, lower cost, often can be loaded immediately.
-
Cons: Not as strong or stable as standard implants; considered a compromise solution. Best for stabilizing lower dentures or replacing small front teeth with low biting force.
-
Cost: $500 – $1,500 per implant.
Zygomatic and Pterygoid Implants
These are extra-long implants used in the upper jaw when there is severe bone loss.
-
How they avoid grafting: They bypass the resorbed jawbone entirely and anchor into the denser, more stable zygomatic (cheek) bone or pterygoid plate.
-
Pros: Eliminates the need for complex sinus lifts and bone grafts. Provides immediate, stable anchorage.
-
Cons: Highly specialized procedure requiring a supremely skilled surgeon. Higher cost and more complex surgery.
-
Cost: The implants and procedure are significantly more expensive than standard implants, often in the $5,000 – $15,000 per arch range.
Bone Expansion (Ridge Expansion)
A technique used when the jawbone is too narrow but not too short.
-
How it avoids grafting: The surgeon uses specialized instruments to gently “crack” and expand the thin ridge of bone, creating enough width to place an implant immediately into the expanded site, often with a small amount of graft material around it.
-
Pros: Can avoid a major block graft surgery.
-
Cons: Only suitable for specific types of bone deficiencies.
Socket Preservation: The Preventative “Graft”
The single best alternative to a major bone graft is to prevent the need for one altogether. If you know you need an extraction, socket preservation is a proactive graft placed at the time of extraction. It is far simpler, less expensive, and more predictable than trying to rebuild bone years later after it has already resorbed.
9. The Cutting Edge: Future Alternatives and Emerging Technologies
The field of regenerative dentistry is advancing rapidly.
-
3D-Printed Bone Grafts: Scientists are developing techniques to 3D print custom, bioresorbable scaffolds that perfectly fit a patient’s defect. These scaffolds can be impregnated with the patient’s own growth factors and stem cells.
-
Gene Therapy and Stem Cell Research: The ultimate goal is to be able to inject signaling factors or stem cells that directly instruct the body to grow new bone on demand, potentially eliminating the need for graft surgery altogether. While still largely in the research phase, this represents the future of the field.
10. Making the Right Choice: A Consultation Checklist
Your consultation is key. Come prepared with questions:
-
What is the exact diagnosis? Can I see my CBCT scan?
-
What type of graft material do you recommend and why?
-
What is your experience with this specific procedure? Can I see before-and-after cases?
-
What is the full, detailed breakdown of the cost? (Surgeon fee, anesthesia, graft material, membrane, facility fee)
-
What is the success rate for this procedure in your practice?
-
What are the specific risks and potential complications for my case?
-
What are the alternatives to a graft, and why are they or aren’t they suitable for me?
-
What does the healing process look like? What are the restrictions?
11. Conclusion
Investing in a dental bone graft is fundamentally an investment in the long-term foundation of your oral health. While the upfront cost and process can seem daunting, it is a highly predictable and successful procedure that enables the placement of durable, functional, and natural-looking dental implants. By understanding the factors that influence price, the types of materials available, and the realistic alternatives, you can move forward with confidence. Partner with a skilled and communicative surgeon to develop a treatment plan that restores not just your smile, but your quality of life, ensuring a stable and healthy result for decades to come.
12. Frequently Asked Questions (FAQs)
Q1: How painful is a dental bone graft?
A: The procedure itself is painless due to anesthesia. Post-operative pain is typically manageable with prescribed or over-the-counter pain medication and is often described as similar to the discomfort after a tooth extraction. Significant pain that worsens after a few days could indicate a complication and should be reported to your surgeon.
Q2: Can a bone graft fail? What causes failure?
A: Yes, though success rates are high (90-95%+). Failure can be caused by:
-
Infection: The most common cause.
-
Poor Blood Supply: The graft fails to integrate if it doesn’t receive adequate blood flow.
-
Patient Factors: Smoking, uncontrolled diabetes, and poor oral hygiene significantly increase the risk of failure.
-
Material Rejection: While rare with modern processing, the body can sometimes reject certain materials.
Q3: How long after a bone graft can I get my implant?
A: The healing and integration period typically ranges from 4 to 9 months, depending on the size and type of graft. A sinus lift often requires the longest healing time (6-9 months). Your surgeon will take a follow-up CBCT scan to confirm the bone is ready before scheduling implant surgery.
Q4: Is it possible to get dental implants without a bone graft?
A: Yes, but only if you have sufficient natural bone volume to support the implant. Many patients who have been missing teeth for a long time do not. Alternatives like zygomatic implants or mini implants may be options in some cases where traditional grafting is not desired.
Q5: How can I avoid needing a bone graft in the future?
A: The best prevention is to address tooth loss quickly. If you need an extraction, always discuss socket preservation with your dentist. This simple, preventative graft at the time of extraction maintains the bone and often eliminates the need for a more complex graft later. Maintaining excellent oral hygiene to prevent periodontal disease is also crucial.
13. Additional Resources
-
American Academy of Periodontology (AAP): www.perio.org – Provides patient information on gum disease and regenerative procedures.
-
American Association of Oral and Maxillofacial Surgeons (AAOMS): www.aaoms.org – A resource for finding a qualified surgeon and understanding oral surgery procedures.
-
International Congress of Oral Implantologists (ICOI): www.icoi.org – A global organization dedicated to providing implant education for both professionals and patients.
-
National Institute of Dental and Craniofacial Research (NIDCR): www.nidcr.nih.gov – Offers information on oral health and ongoing research.
Date: September 16, 2025
Author: Dr. Evelyn Reed, DDS, MS
Disclaimer: This article is for informational purposes only and does not constitute medical advice. The content is not intended to be a substitute for professional medical diagnosis, treatment, or advice. Always seek the advice of your dentist or other qualified health provider with any questions you may have regarding a medical condition or treatment. Prices and technologies mentioned are subject to change and vary by geographic location and individual practice.


