dental code buccal fat pad advancement flap
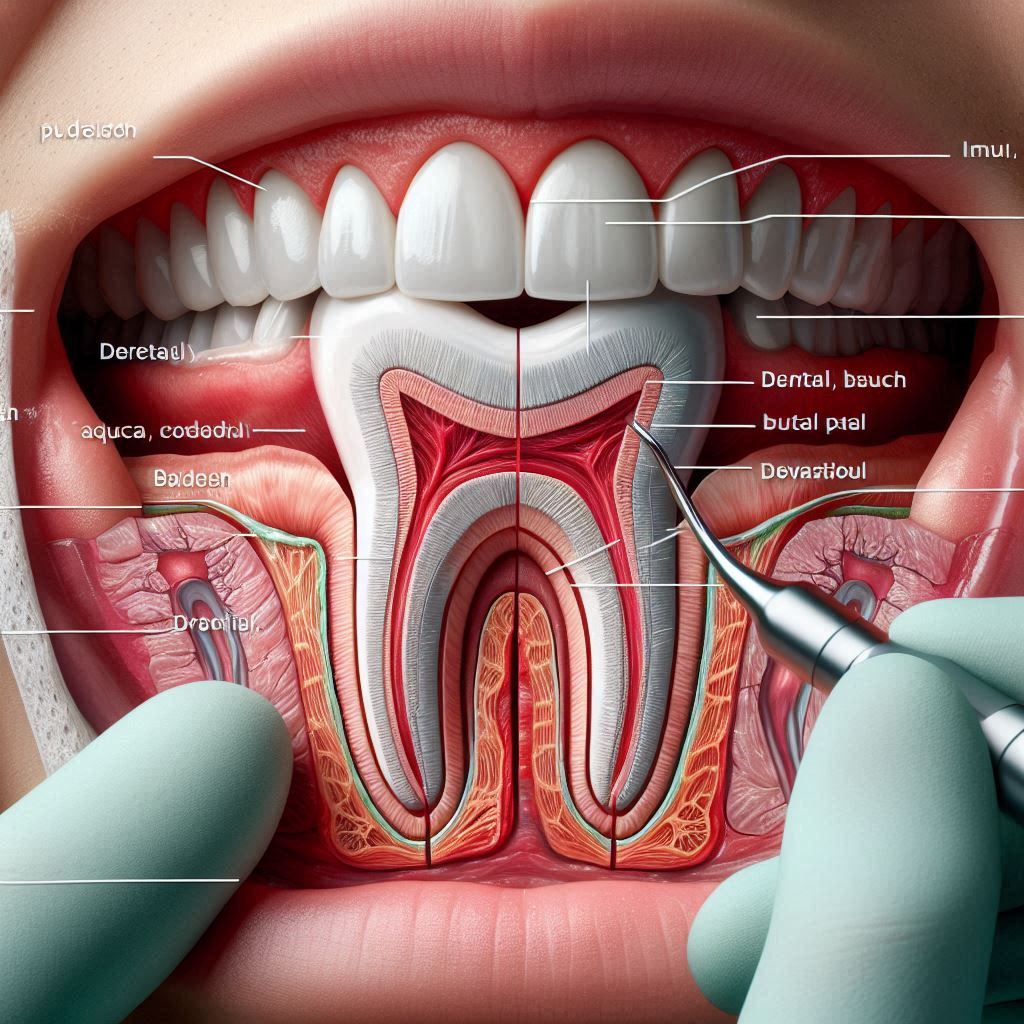
The buccal fat pad (BFP) is a specialized adipose tissue located in the cheek region, playing a crucial role in facial contouring and mastication. Over the years, the buccal fat pad has gained significant attention in the field of oral and maxillofacial surgery, particularly for its use in reconstructive procedures. The buccal fat pad advancement flap is a surgical technique that leverages this fatty tissue to repair oral defects, particularly in the maxillary and mandibular regions. This technique is especially useful in cases where there is a loss of soft tissue due to trauma, tumor resection, or congenital defects.
The buccal fat pad advancement flap is a versatile and reliable method for oral reconstruction. It offers several advantages, including its proximity to the oral cavity, rich blood supply, and minimal donor site morbidity. This article delves into the intricacies of the buccal fat pad advancement flap, covering its dental codes, surgical techniques, clinical applications, and postoperative care.
2. Dental Code for Buccal Fat Pad Advancement Flap: CPT Code
When it comes to billing and coding for the buccal fat pad advancement flap, it is essential to use the correct Current Procedural Terminology (CPT) codes. The CPT code for this procedure is 15740, which is categorized under “Muscle, Myocutaneous, or Fasciocutaneous Flap.” This code is used to describe the surgical transfer of the buccal fat pad to repair oral defects.
Table 1: CPT Codes Related to Buccal Fat Pad Advancement Flap
| CPT Code | Description |
|---|---|
| 15740 | Muscle, Myocutaneous, or Fasciocutaneous Flap; Head and Neck |
| 40816 | Excision of Lesion of Mucosa and Submucosa, Vestibule of Mouth |
| 40818 | Excision of Lesion of Mucosa and Submucosa, Floor of Mouth |
It is crucial for dental and medical professionals to accurately document the procedure to ensure proper reimbursement. The use of the correct CPT code not only facilitates billing but also helps in maintaining a standardized record of the surgical procedure.
3. Buccal Fat Pad Advancement Flap Placement
The placement of the buccal fat pad advancement flap is a meticulous process that requires a thorough understanding of the anatomy of the buccal fat pad and the surrounding structures. The procedure is typically performed under local or general anesthesia, depending on the complexity of the case.
Surgical Technique for Buccal Fat Pad Advancement Flap Placement
- Incision and Exposure: A horizontal incision is made in the buccal mucosa, just above the level of the occlusal plane. The incision is carefully extended to expose the buccal fat pad.
- Mobilization of the Buccal Fat Pad: The buccal fat pad is gently mobilized using blunt dissection. Care is taken to preserve the blood supply to the fat pad, which is crucial for the survival of the flap.
- Advancement and Suturing: The mobilized buccal fat pad is then advanced to cover the defect in the oral cavity. The flap is sutured in place using absorbable sutures, ensuring that the edges are well-approximated.
- Closure: The buccal mucosa is closed over the buccal fat pad, leaving the fat pad exposed in the oral cavity. Over time, the buccal fat pad will epithelialize, providing a stable and functional reconstruction.
Clinical Considerations
- Defect Size: The size of the defect plays a crucial role in determining the feasibility of using the buccal fat pad advancement flap. Larger defects may require additional reconstructive techniques.
- Blood Supply: The buccal fat pad has a rich blood supply, which contributes to its high success rate. However, care must be taken to avoid excessive tension on the flap, which could compromise its vascularity.
4. Buccal Fat Pad Advancement Flap Removal
In some cases, the buccal fat pad advancement flap may need to be removed, either due to complications or as part of a staged surgical procedure. The removal of the buccal fat pad flap is a relatively straightforward procedure, but it requires careful handling to avoid damage to the surrounding tissues.
Surgical Technique for Buccal Fat Pad Advancement Flap Removal
- Incision and Exposure: An incision is made along the previous surgical site to expose the buccal fat pad flap.
- Dissection and Removal: The buccal fat pad flap is carefully dissected from the surrounding tissues. Any adhesions or scar tissue are gently released to facilitate the removal of the flap.
- Closure: Once the buccal fat pad flap has been removed, the buccal mucosa is closed using absorbable sutures. The wound is irrigated to remove any debris, and the area is inspected for any signs of bleeding or infection.
Postoperative Care
- Pain Management: Patients may experience mild to moderate pain following the removal of the buccal fat pad flap. Pain can be managed with over-the-counter analgesics or prescription medications, depending on the severity.
- Oral Hygiene: Patients are advised to maintain good oral hygiene to prevent infection. This includes regular rinsing with an antiseptic mouthwash and avoiding strenuous activities that could disrupt the surgical site.
5. Buccal Fat Pad Advancement Flap Surgery
The buccal fat pad advancement flap surgery is a highly specialized procedure that requires a skilled surgeon with experience in oral and maxillofacial surgery. The surgery is typically performed in a hospital or surgical center, under sterile conditions.
Preoperative Preparation
- Patient Evaluation: A thorough evaluation of the patient’s medical history, including any underlying conditions that could affect the surgery, is essential. Imaging studies, such as CT scans or MRIs, may be performed to assess the extent of the defect and plan the surgery.
- Anesthesia: The type of anesthesia used will depend on the patient’s overall health and the complexity of the procedure. Local anesthesia with sedation is often sufficient for smaller defects, while general anesthesia may be required for larger or more complex cases.
Surgical Procedure
- Incision and Exposure: The surgeon makes an incision in the buccal mucosa to expose the buccal fat pad. The incision is carefully planned to ensure adequate access to the defect.
- Mobilization of the Buccal Fat Pad: The buccal fat pad is mobilized using blunt dissection. The surgeon must be careful to preserve the blood supply to the flap, as this is critical for its survival.
- Advancement and Suturing: The buccal fat pad is advanced to cover the defect and sutured in place. The surgeon ensures that the flap is tension-free and that the edges are well-approximated.
- Closure: The buccal mucosa is closed over the buccal fat pad, leaving the fat pad exposed in the oral cavity. The wound is irrigated, and the surgical site is inspected for any signs of bleeding or infection.
Postoperative Care
- Pain Management: Patients may experience some discomfort following the surgery, which can be managed with pain medications.
- Diet: Patients are advised to follow a soft diet for the first few days after surgery to avoid putting pressure on the surgical site.
- Follow-Up: Regular follow-up appointments are essential to monitor the healing process and address any complications that may arise.
6. Clinical Applications and Case Studies
The buccal fat pad advancement flap has a wide range of clinical applications, making it a valuable tool in the armamentarium of oral and maxillofacial surgeons. Below are some of the most common applications of this technique:
Applications
- Oroantral Fistula Closure: The buccal fat pad advancement flap is commonly used to close oroantral fistulas, which are abnormal connections between the oral cavity and the maxillary sinus.
- Reconstruction After Tumor Resection: The flap is often used to reconstruct defects in the oral cavity following the removal of benign or malignant tumors.
- Trauma Reconstruction: The buccal fat pad can be used to repair soft tissue defects resulting from trauma, such as gunshot wounds or blunt force injuries.
Case Studies
Case Study 1: Oroantral Fistula Closure
A 45-year-old male presented with a chronic oroantral fistula following the extraction of a maxillary molar. The patient had a history of recurrent sinus infections and was experiencing significant discomfort. The decision was made to use a buccal fat pad advancement flap to close the fistula. The surgery was successful, and the patient experienced complete resolution of symptoms with no recurrence.
Case Study 2: Reconstruction After Tumor Resection
A 60-year-old female underwent resection of a benign tumor in the maxillary region, resulting in a large soft tissue defect. A buccal fat pad advancement flap was used to reconstruct the defect. The patient had an uneventful recovery, with excellent functional and aesthetic outcomes.
7. Postoperative Care and Complications
Postoperative Care
- Pain Management: Patients may experience mild to moderate pain following the surgery, which can be managed with analgesics.
- Oral Hygiene: Patients are advised to maintain good oral hygiene to prevent infection. This includes regular rinsing with an antiseptic mouthwash and avoiding strenuous activities that could disrupt the surgical site.
- Diet: A soft diet is recommended for the first few days after surgery to avoid putting pressure on the surgical site.
Complications
- Infection: Although rare, infection can occur following buccal fat pad advancement flap surgery. Signs of infection include redness, swelling, and discharge from the surgical site.
- Flap Necrosis: Flap necrosis is a rare but serious complication that can occur if the blood supply to the flap is compromised. This can result in the loss of the flap and the need for additional reconstructive surgery.
- Scarring: Some patients may experience scarring at the surgical site, although this is usually minimal and does not affect function.
8. FAQs
Q1: What is the buccal fat pad advancement flap?
A: The buccal fat pad advancement flap is a surgical technique that uses the buccal fat pad to repair defects in the oral cavity, particularly in the maxillary and mandibular regions.
Q2: What is the CPT code for buccal fat pad advancement flap surgery?
A: The CPT code for buccal fat pad advancement flap surgery is 15740.
Q3: How long does it take to recover from buccal fat pad advancement flap surgery?
A: Recovery time varies depending on the extent of the surgery, but most patients can expect to recover within 1-2 weeks.
Q4: What are the risks associated with buccal fat pad advancement flap surgery?
A: Risks include infection, flap necrosis, and scarring, although these complications are rare.
Q5: Can the buccal fat pad be used for cosmetic purposes?
A: While the buccal fat pad is primarily used for reconstructive purposes, it has also been used in cosmetic procedures to enhance facial contours.
9. Conclusion
The buccal fat pad advancement flap is a versatile and reliable technique for oral reconstruction, offering numerous advantages, including its proximity to the oral cavity, rich blood supply, and minimal donor site morbidity. With proper surgical technique and postoperative care, the buccal fat pad advancement flap can provide excellent functional and aesthetic outcomes for patients with oral defects.
10. Additional Resources
- American Association of Oral and Maxillofacial Surgeons (AAOMS): https://www.aaoms.org
- American Dental Association (ADA): https://www.ada.org
- Journal of Oral and Maxillofacial Surgery: https://www.joms.org